This is the appendix to the article, “Getting to the Root of the Root Canal Controversy.”
Table of Contents
Toxic Tooth Preface.
It’s Time to Break Down the Wall Between Dentistry and Medicine. By Bruce Donoff MD, DDS (Stat news 2017)
Dental Caries and Head and Neck Cancer (JAMA, 2013)
AAE Newsletters
Jerry Bouquot, DDS, MSD Biographical Profile
Patient Letters to the NYS Dental Board
Weston Price Bio
Articles by Easlick and Grossman that are referenced by the AAE that they say debunks Focal Infection Theory. Current peer reviewed research shows that these articles are filled with false assumptions and outdated information.
Article about Dr. Oz article in response to his critics.
Article: Yes, Licensing Boards Are Cartels. The Case For Why Congress Should Get Involved. By Eric Boehm. Sept. 2017).
Article: The Truth About Dentistry. It’s Much Less Scientific-And More Prone to Gratuitous Procedures-Than You may Think. By Ferris Jabr. The Atlantic. May, 2019).
Article: Root Canal Safety. By Dr. Marcus Johnson. This article is endorsed by the AAE.
More on Stephen Barrett, Jackson Leeds and others.
Appendix
Appendix A: Toxic Tooth Preface
Appendix B:
The belief that oral health is an integral part of total health is gaining momentum. Bruce Donoff, D.M.D.M.D., professor of oral and maxillofacial surgery and dean of the Harvard School of Dental Medicine writes:
“Ever since the first dental school was founded in the United States in 1840, dentistry and medicine have been taught as — and viewed as — two separate professions. That artificial division is bad for the public’s health. It’s time to bring the mouth back into the body. As taught in most schools today, dental education produces good clinicians who have a solid understanding of oral health, but often a more limited perspective on overall health. Few dental students are equipped to take a holistic view that may include taking a patient’s vital signs, evaluating their risk of heart disease or stroke, spotting early warning signs of disease…
My school, the Harvard School of Dental Medicine, was founded 150 years ago on July 17, 1867. It was the first American dental school affiliated with a university and its medical school, and the first to grant the doctor of dental medicine (D.M.D.) degree. The school’s mission is “to develop and foster a community of global leaders dedicated to improving human health by integrating dentistry and medicine at the forefront of education, research, and patient care.” At commencement, dental graduates are welcomed into a “demanding branch of medicine.”…
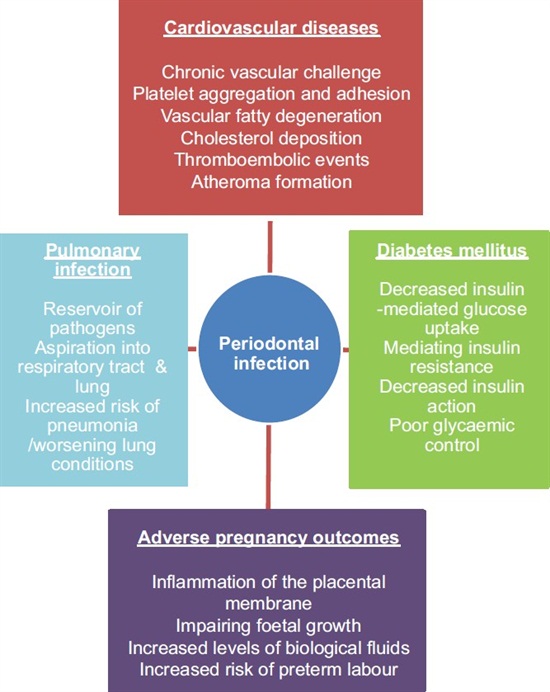
Poor oral health is more than a “tooth problem.” We use our mouth to eat, to breathe, and to speak. Oral pain results in lost time from school and work and lowered self-esteem. Inflammation in the gums and mouth may help set the stage for diabetes, cardiovascular disease, and other chronic conditions. Dental infection can lead to the potentially serious blood infection known as sepsis. In the case of 12-year-old Deamonte Driver, an infected tooth led to a fatal brain infection.
Writing in the Millbank Quarterly, John McDonough, professor of public health practice at the Harvard T.H. Chan School of Public Health asked, “Might oral health be the next big thing?” I believe that it needs to be — and should be.”
The school has also established the Oral Physician Program, a general practice dental residency program at the Cambridge Health Alliance, which integrates oral health, primary care, and family medicine training. We also plan to establish a new combined DMD/MD program with a hospital-based residency to train a new type of physician focused equally on oral health and primary care.
Other institutions are also expanding the concept of dental care and chipping away at the barriers between dental care and primary care. Kaiser Permanente Northwest, for example, has opened a truly integrated medical-dental practice in Eugene, Ore. The Marshfield Clinic in Wisconsin is advancing the concept with integrated medical-dental electronic health records.
Here’s what an integrated dental health/primary care visit might look like to a patient: When you go for a routine teeth cleaning, you would be cared for by a team of physicians, dentists, nurses, and physician and dental assistants. One or more of them would take your blood pressure, check your weight, update your medications, see if you are due for any preventive screenings or treatments, and clean your teeth. If you have an artificial heart valve or have previously had a heart infection, or you are taking a blood thinner, your clinicians will manage these conditions without multiple calls to referring doctors.
Finding the political will to integrate dentistry and primary care is a challenge. Various organizations including the DentaQuest Foundation, the Santa Fe Group, and Oral Health America have taken up the task. The majority of this work is designed to raise awareness of oral health, educate non-dental health care providers, and create political interest in promoting oral health. However, while interprofessional education has met with some success, interprofessional practice remains elusive.
The culture of the dental profession must change to promote closer connections between dentistry and primary care. …
In 2000, the surgeon general’s report “Oral Health in America” drew attention to the gap in oral health in the U.S. In a 2016 update, then-Surgeon General Vivek Murthy strongly recommended integrating oral health and primary care. Closer collaboration between dentistry and primary care could change the culture of health care, close the access gap, and improve general health by providing primary care services during dental visits. It could also improve population health and chronic disease care.
We cannot drill, fill, and extract our way to better oral and overall health. We need a fundamentally different approach, one that accentuates disease prevention and health management using a multidisciplinary, integrated, and patient-centric approach to overall health. And that means breaking down the wall between dentistry and medicine. [Statnews. 2017]
Appendix C:
October 2013
Dental Caries and Head and Neck Cancers
Mine Tezal, DDS, PhD1; Frank A. Scannapieco, DMD, PhD1; Jean Wactawski-Wende, PhD2; et alJukka H. Meurman, MD, PhD3; James R. Marshall, PhD4; Isolde Gina Rojas, DDS, PhD5; Daniel L. Stoler, PhD6; Robert J. Genco, DDS, PhD1
Author Affiliations Article Information
JAMA Otolaryngol Head Neck Surg. 2013;139(10):1054-1060. doi:10.1001/jamaoto.2013.4569
Abstract
Importance Dental caries is the demineralization of tooth structures by lactic acid from fermentation of carbohydrates by commensal gram-positive bacteria. Cariogenic bacteria have been shown to elicit a potent Th1 cytokine polarization and a cell-mediated immune response.
Objective To test the association between dental caries and head and neck squamous cell carcinoma (HNSCC).
Design, Setting, and Participants Case-control study in a comprehensive cancer center including all patients with newly diagnosed primary HNSCC between 1999 and 2007 as cases and all patients without a cancer diagnosis as controls. Those with a history of cancer, dysplasia, or immunodeficiency or who were younger than 21 years were excluded.
Exposures Dental caries, fillings, crowns, and endodontic treatments, measured by the number of affected teeth; missing teeth. We also computed an index variable: decayed, missing, and filled teeth (DMFT).
Main Outcomes and Measures Incident HNSCC.
Results We included 620 participants (399 cases and 221 controls). Cases had a significantly lower mean (SD) number of teeth with caries (1.58 [2.52] vs 2.04 [2.15]; P = .03), crowns (1.27 [2.65] vs 2.10 [3.57]; P = .01), endodontic treatments (0.56 [1.24] vs 1.01 [2.04]; P = .01), and fillings (5.39 [4.31] vs 6.17 [4.51]; P = .04) but more missing teeth (13.71 [10.27] vs 8.50 [8.32]; P < .001) than controls. There was no significant difference in mean DMFT. After adjustment for age at diagnosis, sex, marital status, smoking status, and alcohol use, those in the upper tertiles of caries (odds ratio [OR], 0.32 [95% CI, 0.19-0.55]; P for trend = .001), crowns (OR, 0.46 [95% CI, 0.26-0.84]; P for trend = .03), and endodontic treatments (OR, 0.55 [95% CI, 0.30-1.01]; P for trend = .15) were less likely to have HNSCC than those in the lower tertiles. Missing teeth was no longer associated with HNSCC after adjustment for confounding.
Conclusions and Relevance There is an inverse association between HNSCC and dental caries. This study provides insights for future studies to assess potential beneficial effects of lactic acid bacteria and the associated immune response on HNSCC.
The American Cancer Society predicted an estimated 53 640 new cases of head and neck squamous cell carcinoma (HNSCC) and 11 520 deaths in 2013 in the United States.1 A steady increase in the incidence of oropharyngeal cancers has been observed over the past 3 decades despite a substantial decline in tobacco consumption.2 This increase has been attributed mainly to oral infection with human papillomavirus (HPV) type 16, which was shown to be a causal factor.2 Whereas bacterial colonizations on oral mucosa also differ between healthy individuals and patients with cancer, a causal association between an oral bacterial infection and HNSCC has not been established.3
Dental caries (or decay) and periodontitis are major oral bacterial infections associated with dental plaque.4,5 Although these 2 oral diseases are often combined in a single category as indicators of poor oral health, they are distinct in terms of both etiology and outcome. Periodontitis is a chronic inflammation of structures around the teeth associated with gram-negative anaerobic bacteria leading to alveolar bone loss (ABL).5 It is characterized by Th2 and Th17 polarized immune responses.5In contrast, dental caries results from demineralization of teeth by lactic acid produced from the fermentation of carbohydrates by gram-positive facultative bacteria.4 Cariogenic bacteria are associated with periodontal health, and decreased levels of these commensal bacteria have been shown to be associated with increased periodontal inflammation and destruction.6-8 Multiple studies have shown that dental caries and associated bacteria elicit a potent Th1 immune response in peripheral blood mononuclear cells promoting CD8+ T-cell response.9-11 Whereas Th2 and Th17 cell responses have been generally associated with increased risk of cancer, Th1 cell response has been consistently associated with decreased risk of cancer.12
We previously observed that periodontitis was associated with increased risk of oral potentially malignant disorders13 and HNSCC.14 The purpose of the present study was to test the association between dental caries and HNSCC.
Methods
Study Design and Population
We conducted a case-control study of newly presenting patients of the Department of Dentistry and Maxillofacial Prosthetics at Roswell Park Cancer Institute (RPCI). All patients seen between June 15, 1999, and September 14, 2007, except those who had a history of cancer, dysplasia, or immunodeficiency or were younger than 21 years were included. The RPCI patients come mainly from the surrounding Erie, Niagara, and Chautauqua counties and have a wide range of socioeconomic status. This study was reviewed and approved by institutional review boards of the RPCI and the State University of New York at Buffalo.
Cases
All patients with newly diagnosed primary HNSCC during the study period who met the inclusion criteria were included as cases. The following sites, identified from the RPCI Tumor Registry according to the International Classification of Diseases for Oncology, Third Edition,15 were included: oral cavity, including oral tongue (C02.0-C02.9), gum (C03.0-C03.9), floor of the mouth (C04.0-C04.9), hard palate (C05.0), buccal mucosa (C06.0), vestibule (C06.1), retromolar area (C06.2), and other parts of the mouth (C06.8-C06.9); oropharynx, including base of tongue (C01.0), soft palate (C05.1), tonsil (C09.0-C09.9), and oropharynx (C10.0-C10.9); and larynx (C32.0-C32.9).
Controls
All new patients seen at the department during the same time period as the cases but who did not have a diagnosis of cancer or dysplasia and met the inclusion criteria were included as controls. These included general dentistry patients, as well as those with a diagnosis of benign mucosal lesions such as fibroma, lipoma, wart, traumatic lesion, mucocele, cyst, abscess, pyogenic granuloma, frictional keratosis, and chemical burn. Employees of RPCI were excluded because they represent a different referent population from the one that the cases came from. The diagnoses of controls were obtained from the RPCI Hospital Information System.
Assessment of Oral Variables
The numbers of teeth with caries, fillings, crowns, and endodontic treatments, as well as the severity of periodontitis and missing teeth, were assessed from panoramic radiographs taken at admission before treatment. Severity of periodontitis was assessed according to extent of ABL in millimeters as described previously.14 One examiner blind to cancer status performed all dental measurements. To establish intraexaminer reliability, duplicate measurements were made on 5 randomly selected patients (110 teeth/207 sites). The κ statistics for the numbers of teeth with caries, fillings, crowns, and endodontic treatments and missing teeth were 0.91, 0.96, 1.00, 1.00, and 1.00, respectively. The mean (SD) differences of duplicate ABL measurements were 0.22 (0.41) mm.
Explanatory Variables
Information on the following variables, obtained at the time of diagnosis, was available in patient records: age at diagnosis, sex, race (white, black, Asian, or other), ethnicity (Hispanic or non-Hispanic), marital status (married, single, divorced, widowed, or separated), medical insurance (traditional, Medicare, Medicaid, or uninsured), smoking status (never, former, or current; packs per day), alcohol use (no or yes; drinks per day), tumor stage (I-IV), and tumor differentiation (poor, moderate, well).
Statistical Analysis
Demographic, lifestyle, and clinical characteristics of the study population were summarized by frequency distributions for categorical variables and means with standard deviation for continuous variables. We computed decayed, missing, and filled teeth (DMFT), a widely used measure of caries history.16 To estimate the unadjusted association of HNSCC with dental caries and other exposure variables, crude odds ratios (ORs) and their 95% confidence intervals were calculated from cross-tabulations. Tertiles in the control group were used to categorize exposure variables. The independent association of each exposure variable with HNSCC was estimated from multiple logistic regression analysis. Because of colinearity, each dental variable was evaluated in a separate model. For variable selection, we assessed change in OR when the covariate was added individually to the model. Potential effect modification in the association of dental caries with HNSCC by each covariate was evaluated in stratified analyses and by including multiplicative interaction terms in regression models. A 2-sided P ≤ .05 was considered statistically significant. SPSS Statistics, version 20.0 (IBM), was used for all data analyses.
Results
A total of 620 participants (399 cases and 221 controls) were included. Of the 399 patients with HNSCC, 146 (36.6%) had a diagnosis of oral cavity squamous cell carcinoma (SCC), 151 (37.8%) of oropharyngeal SCC, and 102 (25.6%) of laryngeal SCC. The prevalences of men (P < .001), smokers (P < .001), alcohol users (P < .001), and married participants (P = .01) were significantly higher among cases compared with controls. The cases were significantly older (mean age, 58.62 vs 54.35 years; P < .001), smoked more cigarettes (mean, 0.69 vs 0.30 packs/d; P < .001), and consumed more alcohol (mean, 0.88 vs 0.31 drinks/d; P < .001) compared with controls. The mean numbers of teeth with caries (1.58 vs 2.04; P = .03), endodontic treatments (0.56 vs 1.01; P = .005), crowns (1.27 vs 2.10; P = .004), and fillings (5.39 vs 6.17; P = .04) were significantly lower among cases compared with controls. Conversely, the severity of ABL (mean, 4.03 vs 2.44 mm; P < .001) and the mean numbers of missing teeth (13.71 vs 8.50; P < .001) were significantly higher among cases compared with controls. The cases were not significantly different from controls with respect to race and ethnicity, access to medical insurance, and DMFT (Table 1).
In univariate analyses, participants in the upper tertiles of caries (OR, 0.37 [95% CI, 0.24-0.58]; P for trend <.001), crowns (OR, 0.46 [95% CI, 0.29-0.75]; P for trend = .01), and endodontic treatments (OR, 0.46 [95% CI, 0.28-0.77]; P for trend = .01) were significantly less likely to have HNSCC compared with those in the lower tertiles. Conversely, participants in the upper tertiles of missing teeth (OR, 2.58 [95% CI, 1.73-3.85]; P for trend <.001) and DMFT (OR, 1.58 [95% CI, 1.02-2.44]; P for trend = .06) were significantly more likely to have HNSCC. After adjustment for age at diagnosis, sex, marital status, smoking status, and alcohol use, participants in the upper tertiles of caries (OR, 0.32 [95% CI, 0.19-0.55]; P for trend = .001), crowns (OR, 0.46 [95% CI, 0.26-0.84]; P for trend = .03), and endodontic treatments (OR, 0.55 [95% CI, 0.30-1.01]; P for trend = .15) were less likely to have HNSCC compared with those in the lower tertiles. Missing teeth and DMFT were no longer associated with HNSCC after adjustment for confounding (Table 2).
Stratified analysis by tumor site has shown that dental caries was associated with HNSCC among patients with oral cavity SCC (OR, 0.30 [95% CI, 0.16-0.57]; P for trend <.001) and oropharyngeal SCC (OR, 0.27 [95% CI, 0.13-0.56]; P for trend <.001) but not among those with laryngeal SCC (OR, 0.89 [95% CI, 0.36-2.23]; Pfor trend = .67) (Table 3).
There were no significant interactions between dental caries and any of the other exposure variables. The association between dental caries and HNSCC remained statistically significant among never smokers (OR, 0.27 [95% CI, 0.09-0.79]; P for trend = .05) and never drinkers (OR, 0.35 [95% CI, 0.19-0.67]; P for trend = .04).
Discussion
We observed an inverse association between dental caries and HNSCC, which persisted among never smokers and never drinkers. This association remained significant among patients with oral cavity and oropharyngeal SCC but not among those with laryngeal SCC. Besides untreated caries, 2 other objective measures of long-standing caries history (endodontic treatments and crowns) were also inversely associated with HNSCC with similar effect sizes. This supports the validity of the association between dental caries and HNSCC, suggesting that it is not likely a chance finding. Missing teeth was associated with increased risk of HNSCC in univariate analyses, but after adjustment for potential confounders, its effect was attenuated and was no longer statistically significant.
An increased risk of HNSCC among subjects with periodontitis was reported previously.13,14 To our knowledge, the present study suggests, for the first time, an independent association between dental caries and HNSCC. An inverse association was an unexpected finding because dental caries has been considered a sign of poor oral health. A limited number of previous studies all used composite indices combining dental caries with other oral variables.17-19 Graham et al17 formed a “dentition index” combining decayed, missing, and septic teeth with oral hygiene and condition of prostheses. After adjustment for smoking and alcohol use, inadequate dentition was associated with an increased risk of oral cavity cancer (Mantel-Haenszel relative risk, 3.15; P < .001). Talamini et al18 defined “general oral condition” as a composite index of decayed teeth, tartar, and mucosal irritation. A poor general oral condition was associated with an increased risk of oral cavity and oropharyngeal cancers (OR, 4.5 [95% CI, 1.8-10.9]) after adjustment for age, sex, fruit and vegetable intake, smoking, and alcohol use. In an international study, Guha et al19 defined “general oral health” by the presence of decaying teeth, tartar, gingival bleeding, and mucosal irritation. Poor oral health was associated with an increased risk of HNSCC (oral cavity, pharynx, and larynx) in both central Europe (OR, 2.89 [95% CI, 1.74-4.81]) and Latin America (OR, 1.89 [95% CI, 1.47-2.42]). Because poor oral hygiene, periodontal disease, and missing teeth are all associated with increased risk of HNSCC, an index variable combining these conditions with dental caries will have an apparent positive association with HNSCC, masking the true individual associations.
Mutans streptococci have been suggested as the major cariogenic bacteria, although other acidogenic and aciduric bacterial species including non-mutans streptococci, lactobacilli, actinomycetes, bifidobacteria, and veillonellae also play important roles in the caries process.4 The potential mechanisms by which these commensal bacteria may protect the host from cancer include (1) production of antitumorigenic and antimutagenic compounds; (2) regulation of the cytokine production profile of host cells, promoting cell-mediated response with interferon γ, interleukin 2, interleukin 12, and lymphotoxin α as the prototypic cytokines; (3) production of antimicrobial substances; (4) clearance, inhibition of growth, and downregulation of fimbrial expression of gram-negative bacteria that are potent stimulators of inflammation; (5) production of surfactants; (6) competition with pathogens for adhesion receptors and nutrients; and (7) stabilization of a low pH.20 Interactions between the commensal flora and the host are important for stimulating local mucosal and systemic immunity, tolerance and fine-tuning of T-cell receptor function, epithelial turnover, mucosal vascularity, and lymphoid tissue mass. Dysregulation of such interactions might tip the balance from protective-adaptive to an inflammatory response and result in loss of antitumor effects.20
Supporting our results, a recent study has shown that the prevalence of streptococci in the normal esophagus was significantly higher than that in esophagitis and Barrett esophagus.21 A type 1 microbiome dominated by the genus Streptococcusconcentrated in the normal esophagus, and a type 2 microbiome, characterized by gram-negative anaerobes, was associated with esophagitis and Barrett esophagus. The shift from type 1 to type 2 microbiome was significantly correlated with decreasing levels of streptococci. It has also been shown that patients receiving chemotherapy experience a shift in the oral flora from largely oral streptococci to a more pathogenic gram-negative anaerobic flora that contributes to oral mucositis.22
Whereas caries are localized to tooth surfaces, the commensal cariogenic bacteria are extensively present in saliva and on aerodigestive mucosa. Spread of oral commensals and pathogens to distant body sites by saliva, aspiration, or blood has been demonstrated by many studies.23 Saliva plays an important role in field cancerization by providing a means of transport from 1 surface to another, as well as a means of interaction between different carcinogens.24 In a previous study with the same source population, we had observed that periodontitis, a chronic inflammatory disease, was associated with oral cavity, oropharyngeal, and laryngeal cancers.14 In the present study, dental caries was associated with HNSCC among patients with oral cavity and oropharyngeal cancers but not among those with laryngeal cancers. Almost all patients with laryngeal cancer (98%) had a history of smoking, compared with 76% and 78% of patients with oral cavity and oropharyngeal cancers. They also consumed significantly greater amounts of tobacco and alcohol, were older, and had more missing teeth.
The number of missing teeth was associated with increased HNSCC risk in univariate analysis, but its effect size was attenuated and lost statistical significance after adjustment for explanatory variables. Whereas few previous studies reported a positive association between tooth loss and HNSCC,25-27 most studies, similar to ours, reported a nonsignificant association after adjustment for confounding.18,19,28,29 Missing teeth can be misleading as a surrogate measure for caries or periodontitis when their relationships with HNSCC are assessed because the etiologies, as well as the outcomes, of these 2 diseases are very different. Because periodontitis is associated with an increased risk of HNSCC, the risk will increase proportional to the number of affected teeth. Conversely, if dental caries is inversely associated with HNSCC, the risk will decrease proportional to the number of affected teeth. Therefore, the association between missing teeth and HNSCC depends on the reason for tooth loss. The number of DMFT was also not associated with HNSCC in the present study, which was not a surprise. The number of DMFT is a measure of dental caries with a long record of use in the literature and is widely accepted around the world.16 However, it is a composite index combining untreated dental caries with missing teeth and fillings, and for the reasons discussed here, it does not represent dental caries history accurately.
Missing teeth is a difficult issue to deal with especially in retrospective studies when the reason for tooth loss is unknown. In our initial analyses, we assessed the effect of missing teeth as a potential confounder and an effect modifier. Dental caries was not significantly correlated with missing teeth (r = −0.012). When missing teeth was added as a covariate to the model, the change in the main effect estimate (OR) was only 0.02, suggesting that missing teeth was not a significant confounder. In addition, potential effect modification by missing teeth was evaluated in stratified analyses and by including an interaction term in the multiple logistic regression. There was no significant interaction between missing teeth and caries (P = .77). The association between dental caries and HNSCC remained significant in subjects with low, moderate, and high numbers of missing teeth (categorized by tertiles) with similar effect sizes in all strata.
The present study analyzed existing data, and the information on certain potential confounders, including socioeconomic status (SES), diet, and HPV status was not available. The SES variables are highly correlated with each other, with higher education usually leading to higher income, better residence, and better health insurance.30,31 Therefore, surrogate variables of SES, such as zip code or medical or dental insurance, may be used when data on traditional SES variables such as education and income are not available. In the present study, the only standard SES variable available for all study participants was medical insurance, and 51.5% had employer-sponsored insurance, 33.7% had Medicare, 10.3% had Medicaid, and 4.5% were uninsured. According to the Census Bureau’s 2011 Current Population Survey, 55.3% of the US general population is covered by employer-sponsored insurance, 14.5% by Medicare, 15.9% by Medicaid, and 16.3% is uninsured.31 Although the proportions of employer-sponsored insurance and Medicaid in our study population were similar to those of the general US population, the proportion of subjects with Medicare was higher and the proportion of uninsured subjects was lower. This is expected because our study population is hospital-based and older.
Frequent consumption of sugar is an important factor in the etiology of dental caries.4 On the other hand, an inverse association between fruit and vegetable intake and the risk of HNSCC is well established.17,20 It is likely that sugar and acid in fruits contributed to the higher frequency of dental caries in controls while lowering their risk of HNSCC. Therefore, the role of diet in the association between dental caries and HNSCC needs to be assessed in future studies.
Data regarding HPV status were available for a subset of patients with cancer. Among 125 patients with known HPV status, the mean numbers of teeth with dental caries (1.37 vs 1.86; P = .37), fillings (5.25 vs 5.40; P = .86), endodontic treatments (0.46 vs 0.57; P = .63), and crowns (0.90 vs 0.93; P = .95) were not significantly different in patients with HPV-negative and HPV-positive tumors, suggesting that HPV is not likely to influence the effect estimate. In addition, there is no known association between dental caries and oral HPV infection.
Another limitation of the study is that detailed data on dental caries, including their depth and location, were not available. It is known that radiographs underestimate the frequency and extent of dental caries, especially in early stages.32However, because the same methods were used for cases and controls and all measurements were performed by 1 examiner blind to cancer status, the measurement bias is not likely to be significant and would only lead to underestimation of the true effect.33 The radiographs from which dental caries was assessed were obtained at the time of diagnosis before cancer treatment was initiated. Dental caries is a chronic disease, which starts and progresses slowly, and detectable dental caries on radiographs reflects preexisting disease history. Therefore, despite the case-control design of the present study, existing data provide evidence of temporality that dental caries preceded cancer diagnosis.
An important strength of the present study is that the cases and controls were selected from the same source population, the same way. All case and control patients with new diagnoses who met the inclusion criteria during the study period were included without knowledge of their dental status. Therefore, the selection bias in this study is also not likely to be significant.33
Although the importance of the local environment for carcinogenesis is widely accepted, research evaluating the role of oral factors in the natural history of HNSCC is lacking. If confirmed by other studies, the findings of this study have important implications for the management of HNSCC, as well as oral infections. It is important to remember that the majority of commensal bacteria are beneficial to the host, and streptococci are the most abundant genus in the oral cavity (52%).34Cariogenic bacteria are part of the commensal oral flora, and their presence is not sufficient to cause dental caries in the absence of the other risk factors, such as dental plaque, frequent consumption of a carbohydrate-rich diet, and reduced saliva production.4 Caries is a dental plaque–related disease. Lactic acid bacteria cause demineralization (caries) only when they are in dental plaque in immediate contact with the tooth surface. The presence of these otherwise beneficial bacteria in saliva or on mucosal surfaces may protect the host against chronic inflammatory diseases and HNSCC. We could think of dental caries as a form of collateral damageand develop strategies to reduce its risk while preserving the beneficial effects of the lactic acid bacteria. For example, antimicrobial treatment, vaccination, or gene therapy against cariogenic bacteria may lead to more harm than benefit in the long run, including a shift in microbial ecology toward gram-negative bacteria and increased risks of chronic inflammatory diseases and cancer. Instead, strategies preserving microbial ecology beneficial to the host such as mechanical plaque control, preservation of saliva, and use of fluoride, as well as control of diet and other risk factors, might be wiser. Future studies assessing the potential effects of the oral microbiome and associated immune responses on HNSCC will help elucidate the biological mechanism of the clinical association that we have observed in this study.
Article Information
Corresponding Author: Mine Tezal, DDS, PhD, State University of New York at Buffalo, 202 Foster Hall, Buffalo, NY 14214 (mtezal@buffalo.edu).
Submitted for Publication: April 3, 2013; final revision received June 18, 2013; accepted July 22, 2013.
Published Online: September 12, 2013. doi:10.1001/jamaoto.2013.4569.
Appendix D:
These are two newsletters published by the AAE. Current research directly contradicts some of the statements and assumptions presented in these newsletters.
Compare what the AAE states in these newsletters to the actual peer reviewed scientific article presented and see what is true, what is misleading, and what is completely false in these AAE newsletters.
Selected References for Spring/Summer 2000
ENDODONTICS: Colleagues for Excellence
Oral disease and systemic health: What is the connection?
American Association of Endodontists. Root canal therapy safe and effective, Endodontics: Colleagues for Excellence. F/W 1994.
American Heart Association recommendations. Prevention of bacterial endocarditis, JAMA 1997;227:1794-1801.
Baumgartner, J C et al. The incidence of bacteremias related to endodontic procedures I. Nonsurgical endodontics J Endodon, 1976;2:135-140.
American Association of Endodontists, The incidence of bacteremia in endodontic manipulation – preliminary report Oral Surg Oral Med Oral Pathol, 1960;
Peters, LB et al, The fate and the role of bacteria left in root dentinal tubules, Int Endod J, 1995;28:95-99.
American Academy of Periodontology Periodontal disease as a potential risk factor for systemic diseases J Periodontology 1998;69:841-850.
Beck J et al, Periodontal disease and cardiovascular disease, J Periodontology 1996;67:1123-1137.
Offenbacher, S et al, Periodontal infection as a possible risk factor for preterm low birth weight, J Periodontology 1996;67:1103-1113.
Slots, J Casual or causal relationship between periodontal infection and non-oral disease? J Dent Res 1998;77:10.
Herzber MC and Meyer MW Effects of oral flora on platelets: Possible consequences in cardiovascular disease, J Periodontology 1996;67:1138-1142.
Grossman LI, Root Canal Therapy. 4th Edition. Lea & Febiger, Philadelphia. pp. 18-24, 1940.
Appendix E:
Biographical profile of Jerry Bouquot, DDS, MSD.
Dr. Jerry Bouquot earned his DDS and MSD degrees from the University of Minnesota, with postdoctoral fellowships to the Mayo Clinic and the Royal Dental College in Copenhagen, Denmark as the recipient of a Career Development Award from the American Cancer Society.
He holds the record as the youngest oral pathology chair in U.S. history and for more than 26 years was chair of two diagnostic science departments, one in West Virginia University and the other at The University of Texas Health Science Center at Houston.
He has received more than 50 honors and awards, including WVU’s highest awards for teaching and service to humanity, and its alumni association’s Lifetime Achievement Award. He received the St. George National Award, the highest award given by the American Cancer Society for lifetime efforts in cancer control, and has been awarded the Bridgeman Distinguished Dentist Award from the West Virginia Dental Association, the Distinguished Leadership Award from the West Virginia Public Health Association, a Presidential Certificate of Appreciation from the American Academy of Oral Medicine, Honorary Life Membership from the International Association of Oral Pathologists, the Distinguished Alumnus Award from the University of Minnesota and both the Fleming and Davenport Award for Original Research and the Award for Pioneer Work in Teaching & Research from The University of Texas.
He is now a retired adjunct professor of The University of Texas and West Virginia University, and remains the director of research for his private research center, the Maxillofacial Center for Education and Research.
He has been director of two of the largest U.S. oral pathology biopsy services, one of which received tissue from 45 states and five foreign countries. He has been the dental director of the West Virginia Bureau for Public Health, a Senior Visiting Scientist of the Mayo Clinic, a Special Advisor to the National Institutes of Health, an Honorary Member of Dental Informatics of the University of Göteborg, Sweden, a Gorlin Visiting Professor of the University of Minnesota, and the Oral Cancer Control Coordinator for the state of West Virginia.
He has been a consultant to Pittsburgh Children's Hospital and the New York Eye & Ear Infirmary. He has been awarded Fellowship in the International College of Dentists, the American College of Dentists, the Academy of Dentistry International, the American Academy of Oral & Maxillofacial Pathology and the Royal Society of Medicine (U.K.); he has been on the Scientific Advisory Boards of four U.S. and European corporations. During his career, he peer-reviewed more than 1,500 scientific papers for more than 40 journals.
Dr. Bouquot has more than 340 published papers, abstracts, books and book chapters. His work has been translated into numerous languages, has been cited more than 6,000 times in the literature, and has been used by state and national governments to determine oral health policy.
He is co-author of the most popular textbook of oral pathology, has named more than three dozen oral diseases, has been a reviewer for more than 40 medical and dental journals, and has been on the editorial boards of four international dental journals. He has presented more than 1,600 research and continuing education seminars in more than 30 countries and all 50 U.S. states, and has taught what are possibly the longest-running community-based CE courses in U.S. dentistry. His informational websites are the two most popular oral pathology sites on the internet, together getting almost 6.5 million hits annually.
Dr. Bouquot is a past president of the American Board of Oral & Maxillofacial Pathology, the Eastern Society of Teachers of Oral Pathology, the Western Society of Teachers of Oral Pathology, the Organization of Teachers of Oral Diagnosis, four regional dental societies, and the West Virginia Division of the American Cancer Society. He has been a member of the Executive Council of the American Academy of Oral & Maxillofacial Pathology, the national Board of Directors of the ACS and the Board of Trustees for the eight-state South Atlantic Division of the ACS. As a member of the ACS National Research Committee, he was among those responsible for reviewing and approving more than $90 million in cancer research grants annually.
Board Certification
American Board of Oral & Maxillofacial Pathology
APPENDIX F:
APPENDIX G: Weston Price Bio
APPENDIX H: Easlick and Grossman references used by the AAE. I believe that it is important to see the actual articles used to refute focal infection and see how they hold up to current peer reviewed research.
Some of the assumptions used by Easlick and Grossman to debunk focal infection have since been proven false and therefore do not debunk focal infection.
Interestingly, the AAE cites these two studies and authors as their number one and number two references on the safety of root canal teeth.
APPENDIX I:
Dr. Oz Is No Wizard, but No Quack, Either
By Bill Gifford
April 25, 2015
ONE afternoon last December, my book publicist called with the best possible news: “You’re booked on ‘The Dr. Oz Show’!” she crowed. This was a huge coup, and I tried to sound as thrilled as she was.
Secretly, my heart sank. Dr. Oz? As a serious science writer and devout skeptic, I knew I was supposed to scorn him.
He’d been savaged on social media for months. Last June, Senator Claire McCaskill, Democrat of Missouri, had given him a public tongue-lashing for touting a supplement called green coffee bean extract, which he had called “a magic weight loss cure for every body type,” among other over-the-top statements. His enthusiasm was based on a single small study that later turned out to be bogus, and was eventually retracted. Oops. His critics had a field day.
Then, in December, The BMJ, a British medical journal, published a study claiming that fewer than half of the on-air recommendations on “The Dr. Oz Show” were supported by scientific evidence. I happened to be taping my segment that day, and my new pal, Dr. Oz, seemed rather tense. When I said something positive about the health benefits of red wine, he remarked sardonically, “That’s good, because I talk about it all the time.”
Earlier this month, a group of 10 self-described “distinguished physicians” piled on with a letter urging Columbia University to fire Dr. Mehmet Oz from his post as vice chairman of the department of surgery. “Dr. Oz has repeatedly shown disdain for science and for evidence-based medicine,” they wrote. “Worst of all,” they went on, “he has manifested an egregious lack of integrity by promoting quack treatments and cures in the interest of personal financial gain.”
On Thursday, an indignant Dr. Oz fired back, saying that he does not endorse or profit from the products he promotes. He also went after his critics personally. Several have ties to an industry-funded advocacy group, he noted, and one — Dr. Gilbert Ross — did prison time for Medicaid fraud, which is an odd definition of “distinguished.”
The ad hominem exchange was unfortunate. A more careful look, however, at the merits of the supposed case against him makes it start to look weaker than a cup of green coffee.
That BMJ study, for example: When researchers analyzed 80 “randomly selected” recommendations from “The Dr. Oz Show,” they judged that 26 of them, or 33 percent, were supported by evidence they deemed “believable.” They found just nine recommendations that were contradicted by convincing scientific literature. Looked at this way, Dr. Oz is proved wrong only 11 percent of the time — not ideal but hardly “egregious.” The BMJ authors also didn’t list the statements they examined and the evidence for or against, so it’s hard to know how serious these errors might have been.
The show on which I appeared aired on Feb. 19, and it featured the author of “The Bra Book,” and the story of a woman who didn’t know she was pregnant until shortly before she gave birth. The comedian Wanda Sykes talked about hot flashes, some women did yoga-type exercises, and there was a segment on “back boobs,” whatever those are.
It was a surreal experience, but this is what Dr. Oz does. He covers health-related subjects — like bowel movements, menopause and body fat — that many people find awkward to discuss, even taboo. Much of what Dr. Oz talks about is pretty anodyne stuff: Eat fruit! Exercise! Sleep right! Diet features prominently on every show: The celebrity chef Rocco DiSpirito demonstrated supposed fat-burning recipes on the show in which my segment appeared.
It’s hard to complain about a guy advising American families on how to cook healthier meals. Do we really need double-blind clinical trials of Mr. DiSpirito’s recipes? Must “The Bra Book” be submitted for peer review? This is daytime television, not the Journal of the American Medical Association.
Yet these are not things that you’ll hear much about in a typical 15-minute visit to your doctor. Despite mounting evidence that diet is crucial to health, most medical schools offer only rudimentary training in nutrition. A 2011 study found that only 45 percent of overweight patients had been alerted to the fact by their doctors. For obese patients, the figure was even worse: Nearly two-thirds hadn’t gotten this message. Given the overwhelming evidence on the health hazards of obesity, shouldn’t it be more like 100 percent?
The doctors’ letter raises an interesting question: Is “evidence-based medicine” itself always a settled issue? In scientific inquiry, the “truth” is slipperier and more fluid than distinguished physicians will generally admit. Different doctors take different approaches to issues like whether or not to prescribe statin drugs to patients with high cholesterol, or how to treat people with pre-diabetes.
Some are quick to prescribe medications, whereas Dr. Oz tends to favor less interventionist, more natural approaches based on diet and exercise. Again, hard to see the problem there — especially in the context of a television show when direct-to-consumer advertising of pharmaceuticals pervades the airwaves. (The only other country that permits marketing like this is New Zealand.)
One of the products frequently advertised on TV, for example, is testosterone replacement therapy, for a condition called “low T.” In March, the Food and Drug Administration issued a stern warning to physicians and makers of “low T” treatments, saying the medications have been overprescribed for age-related applications and could lead to an increased risk of stroke and cardiovascular problems. Dr. Oz, meanwhile, has devoted more than one segment to exploring natural ways to deal with “low T” symptoms like low energy, poor sex drive, weight gain and depression.
A diversity of medical opinion is not a bad thing; in fact, far from it. Today’s fringe treatments could well become tomorrow’s standard protocol.
For example, the American Heart Association’s cholesterol guidelines focus on the “good” and “bad” types of cholesterol (H.D.L. and L.D.L., respectively). But this largely ignores another biological marker, a lipoprotein known as ApoB, which a growing body of research has shown to be a much better predictor of heart disease risk. The evidence points in a new direction, yet the A.H.A. guidelines lag behind.
Progress in medicine and science is a messy, contested affair. It can be hard to know who’s right or wrong until the dust has settled and time has passed. Without people pushing the boundaries of accepted treatments and conventional wisdom — and fostering dialogue, which Dr. Oz sees as part of his mission — there would be no advancement.
Here in America, rightly or wrongly, we have clearly chosen a wild and woolly marketplace where free speech comes before regulation and expert ruling. That means that, as patients and consumers, we need to do our own homework and exercise another precious right: the right to a second opinion. And then, maybe, a third.
APPENDIX J
Remembering Roger Boisjoly: He Tried To Stop Shuttle Challenger Launch
By Howard Berkes 2012
Roger Boisjoly was a booster rocket engineer at NASA contractor Morton Thiokol in Utah in January, 1986, when he and four colleagues became embroiled in the fatal decision to launch the Space Shuttle Challenger.
Boisjoly was also one of two confidential sources quoted by NPR three weeks later in the first detailed report about the Challenger launch decision, and the stiff resistance by Boisjoly and other Thiokol engineers.
The experience both haunted and inspired Boisjoly in the decades that followed. We learned this weekend from this story in The New York Times that Boisjoly died last month in Utah at age 73.
Bulky, bald and tall, Boisjoly was an imposing figure, especially when armed with data. He found disturbing the data he reviewed about the booster rockets that would lift Challenger into space. Six months before the Challenger explosion, he predicted "a catastrophe of the highest order" involving "loss of human life" in a memo to managers at Thiokol.
The problem, Boisjoly wrote, was the elastic seals at the joints of the multi-stage booster rockets. They tended to stiffen and unseal in cold weather and NASA's ambitious shuttle launch schedule included winter lift-offs with risky temperatures, even in Florida.
On January 27, 1986, the forecast for the next morning at the Kennedy Space Center included a launch-time temperature as low as 30 degrees Fahrenheit. NASA had never launched in temperatures that cold and Boisjoly and his four colleagues at Thiokol headquarters in Utah concluded it would be too dangerous too launch.
Three weeks later, he told NPR's Daniel Zwerdling in an unrecorded and confidential interview, "I fought like Hell to stop that launch. I'm so torn up inside I can hardly talk about it, even now."
But Boisjoly did talk about it in a hotel room in Alabama, revealing for the first time the details of that effort to keep Challenger on the launch pad. He asked that he not be named but he agreed to be quoted anonymously. As he spoke with Zwerdling, a second engineer revealed the same details to me under the same conditions at his home in Brigham City, Utah.
Boisjoly's family agreed to release him from our pledge of confidentiality so that his efforts to get the truth out can be widely known.
"We all knew what the implication was without actually coming out and saying it," a tearful Boisjoly told Zwerdling in 1986. "We all knew if the seals failed the shuttle would blow up."
Armed with the data that described that possibility, Boisjoly and his colleagues argued persistently and vigorously for hours. At first, Thiokol managers agreed with them and formally recommended a launch delay. But NASA officials on a conference call challenged that recommendation.
"I am appalled," said NASA's George Hardy, according to Boisjoly and our other source in the room. "I am appalled by your recommendation."
Another shuttle program manager, Lawrence Mulloy, didn't hide his disdain. "My God, Thiokol," he said. "When do you want me to launch — next April?"
These words and this debate were not known publicly until our interviews with Boisjoly and his colleague. They told us that the NASA pressure caused Thiokol managers to "put their management hats on," as one source told us. They overruled Boisjoly and the other engineers and told NASA to go ahead and launch.
"We thought that if the seals failed the shuttle would never get off the launch pad," Boisjoly told Zwerdling. So, when Challenger lifted off without incident, he and the others watching television screens at Thiokol's Utah plant were relieved.
"And when we were one minute into the launch a friend turned to me and said, 'Oh God. We made it. We made it!'" Boisjoly continued. "Then, a few seconds later, the shuttle blew up. And we all knew exactly what happened."
Until NPR's story, the special commission investigating the Challenger tragedy hadn't even interviewed all the engineers involved in the pre-launch debate.
The explosion of Challenger and the deaths of its crew, including Teacher-in Space Christa McAuliffe, traumatized the nation and left Boisjoly disabled by severe headaches, steeped in depression and unable to sleep. When I visited him at his Utah home in April of 1987, he was thin, tearful and tense. He huddled in the corner of a couch, his arms tightly folded on his chest. But he was ready to speak publicly.
"I'm very angry that nobody listened," Boisjoly told me. And he asked himself, he said, if he could have done anything different. But then a flash of certainty returned.
"We were talking to the right people," he said. "We were talking to the people who had the power to stop that launch."
Boisjoly testified before the Challenger Commission and filed unsuccessful lawsuits against Thiokol and NASA. He continued to suffer and was ostracized by some of his colleagues. One said he'd drop his kids on Boisjoly's doorstep if they all lost their jobs, according to his wife Roberta.
"He took it very hard," she recalls. "He had always been held in such high esteem and it hurt so bad when they wouldn't listen to him."
A therapist recommended speaking out even more and for close to three decades, Boisjoly traveled to engineering schools around the world, speaking about ethical decision-making and sticking with data. "This is what I was meant to do," he told Roberta, "to have impact on young people's lives."
Boisjoly continued to respond to emails and letters from engineering students right up until his sudden death in his sleep last month in St. George, Utah. He was diagnosed with cancer two weeks before.
"He always stood by his work," Roberta recalls, her voice breaking. "He lived an honorable and ethical life. And he was at peace when he died."
Challenger's Whistle-Blower: Hero And Outcast
The engineer who opposed the doomed launching of the shuttle finds himself ostracized as he embarks on several new careers. PHOENIX--When the shuttle Challenger blew up, the explosion lit a fuse in Roger Boisjoly's conscience. A structural engineer for Morton Thiokol Inc., the firm that later bore blame for the disaster, Boisjoly had argued against the launch the night before and, like the rest of the nation, watched in horror when the shuttle blew up. "I left the room and went directly to my
Jan 20, 1990
ELIZABETH PENNISI
5
The engineer who opposed the doomed launching of the shuttle finds himself ostracized as he embarks on several new careers.
|
PHOENIX--When the shuttle Challenger blew up, the explosion lit a fuse in Roger Boisjoly's conscience. A structural engineer for Morton Thiokol Inc., the firm that later bore blame for the disaster, Boisjoly had argued against the launch the night before and, like the rest of the nation, watched in horror when the shuttle blew up. "I left the room and went directly to my office where I remained in shock the rest of the day," he recalls about that terrible morning four years ago this week.
During the next eight months, Boisjoly would become both a national hero and a professional pariah. Although widely lauded for his courage in alerting the National Aeronautics and Space Administration and his company to the dangers in the design of the space vehicle's booster rockets and for his frank testimony to a presidential commission investigating the accident, he has paid a terrible personal price for his actions. He was ostracized by most of the 1,600 residents of Willard, Utah, where Morton Thiokol is based and where, just three years earlier, he had served as mayor. And his life at Morton Thiokol, which made the faulty booster rockets, became unbearable.
"He acted to protect the public interest at a significant cost to his health and professional well-being," says Mark Frankel, head of the scientific freedom and responsibility program at the American Association for the Advancement of Science, which gave Boisjoly its annual award in 1988. "He made every effort to act responsibly, and for that he has paid a high price."
Now Boisjoly and his wife live in Mesa, Ariz., a suburb of Phoenix. He has set up his own consulting business and hopes to work primarily for lawyers, as a technical expert. His business card states his philosophy, as well as his place in history: "Vigorously Opposed Launching Space Shuttle Challenger."
Over these past four years Boisjoly has wrestled daily with an issue that all scientists fear but few have to face: When does one speak out? And at what price to one's career? And to one's company? As an engineer, Boisjoly might put it in more technical terms: How does one determine the appropriate risk of one's actions?
As a consultant for General Motors, Ron Westrum is trying to stimulate creativity within a corporate structure. Last year, he decided that Roger Boisjoly should be one of his program's key speakers. "I'm sure that in many corporations, somebody like Roger would have been looked down upon," says Westrum, a professor of sociology and interdisciplinary technology at Eastern Michigan University in Ypsilanti. "But we're trying to change that." Westrum respects Boisjoly's honesty, openness, and courage, and he hopes that the lessons from the Challenger accident will encourage employees to speak out when they see a problem and help managers to be more receptive to those comments. "If companies tend to dismiss information about danger, then they are also likely to dismiss information about innovation," says Westrum. Boisjoly's lectures generally trace the details leading up to the final meeting before the scheduled launch of the Challenger. In the meeting Morton Thiokol executives capitulated to pressure from NASA and gave their assent to the launch despite concerns from engineers about the effect of the freezing temperatures on the seals of the booster rocket. It is not enough for engineers to be able to assess risk, Boisjoly tells his audiences. If there is danger of injury or loss of life, an engineer must be able to communicate that risk and work to prevent damage. He recounts how he tried to raise the red flag, first by working within his company through memos to his superiors and, later, through direct warnings to NASA, the customer. The memos went unheeded, and his objections were overruled. His standards for assessing risk are high, perhaps higher than corporate planners can justify. But he sees no alternative, and the Challenger accident bears out his worse fears. Despite his concerns, he reminds himself, the launch proceeded. He has turned that experience into a campaign for stronger professional ethics and for the need to speak out against risk. He visits college campuses about twice a month, where his message is well-received. "The students see him as a role model," says William Middleton, chairman of the ethics committee for IEEE USA. "I think he will do a great deal to change the ethical perspective [of future engineers]." Westrum and others think Boisjoly has a broader message as well. "It's very important for high-technology firms to do what they can to speed the flow of technological information," he says. "Roger has a lot to say about why information did not flow." MIT officials have also invited him to talk to students - not about Challenger, but about what it's like to be an engineer in a big corporation. In the coming months he will visit a second General Motors plant and at least one other corporation. It's essential that information flow smoothly and that corporations listen more closely to people like Boisjoly, Westrum asserts. "If they don't," he warns, "this country will continue to go down the tubes." --E.P. |
Not surprisingly, his former employer does not share Boisjoly's eagerness to discuss his actions and their meaning. A spokesman for Morton Thiokol declined to comment on any matter relating to Boisjoly, saying that the subject is closed. But colleagues applaud Boisjoly's efforts to raise the issue of professional ethics and to stress its importance.
"He's one of a very small group of people who have had the courage of their convictions," says William Middleton, chairman of the ethics committee for the Institute of Electrical and Electronics Engineers (IEEE). "He took the matter into his own hands and dealt with it by going public on a whistle-blowing campaign. And now he's sort of blacklisted. To those of us who do work in the ethics area, he's a hero."
Boisjoly, now 51, had no idea he would ever play such a role when he went to work for Morton Thiokol in 1980 as a structural engineer. His job then was to analyze the cases that enclosed the space shuttle's solid rocket boosters. He used data from past flights to generate flight-readiness updates for NASA, and eventually became a technical trouble- shooter for the company.
In late 1985, he became one of five engineers in charge of redesigning the seals and joints on the booster rockets. He became increasingly concerned about the ability of the seals to work properly at extreme temperatures. Although he passed his worries along to his managers, the problems were never given a high priority.
On the night before the January 1986 launch, Florida experienced a statewide cold snap. The weather prompted a teleconference between NASA and Morton Thiokol that ended, despite the engineers' objections, in a decision to go ahead with the launch. Boisjoly's subsequent testimony to a presidential commission and later to Congress helped government investigators learn about the process that contributed to the tragedy. He and two other engineers helped interpret the technical data for the committees and were more willing than Morton Thiokol to provide details of the events leading up to the launch.
Following the disaster, Boisjoly stayed on at Morton Thiokol as a senior engineer involved in redesigning the faulty seals. But he says he was not allowed to interact with NASA, nor was he given much responsibility by his superiors. "Instead," he recalls, "they put me through hell on a day-to-day basis." He became sick and depressed, a condition that doctors diagnosed as posttraumatic stress disorder. In June 1986, after testifying before Congress, he stopped going to work and went on extended sick leave. In January 1987 he began receiving long-term disability pay, collecting 60% of his salary until the benefits ran out in January 1989.
Now he's hopeful that his integrity, knowledge, and experience will attract clients to his fledgling consulting practice. "Attorneys that care and do stand for facts will want me," Boisjoly asserts.
Few engineers can match Boisjoly's track record of testifying under pressure. He was also grilled by FBI agents and officials from the Justice Department about his work analyzing technical data. "They were asking hard questions about what really happened," he recalls.
"It's engineering work plus what a lot of people cannot do - get up and communicate your findings in an adversarial environment."
Boisjoly has registered with two services that provide expert witnesses to attorneys, and he's paid to have his name added to a national directory. Last summer he sent handwritten notes to a dozen editors and reporters who had interviewed him, asking them for referrals. As a consultant he plans to provide lay interpretations of technical specifications and can determine whether a product meets the required standards. "It's just a matter of getting a match and showing people what I can do," he says.
But, so far, Roger Boisjoly's unique brand of engineering expertise is not much in demand. It takes time, he says, for lawyers to get to know what he has to offer. He did one day's worth of work examining a product that failed on a helicopter, and he's fielded a few calls from prospective clients. He fills the hours by revising his talk, making telephone calls, and puttering about the house. He's also written a few magazine articles and a technical paper for the American Society of Civil Engineers.
"The hardest part is getting over the frustration of knowing that we are barely eking out an existence while waiting for something to happen," he says. "I think there is a limit to how much a human being can take." In the meantime, his wife stays busy helping her daughter with a new baby, and the two of them are getting to know their neighbors.
Boisjoly is most visible on the college lecture circuit. He's given more than 70 talks in the United States, Canada, and Norway about his role in the accident and the investigation, and he still visits campuses about twice a month.
Until recently, his fees from speaking engagements barely covered his expenses, and the talks were chiefly therapeutic. Now they are a financial necessity, he says. "It's these talks and the honoraria that keep us floating."
His peers also appreciate his message. In 1988 he spoke to the American Society of Mechanical Engineers to pick up that group's Founders Award. A year earlier the National Space Society cited him with its presidential award. He has also been honored by IEEE USA.
The reaction to Boisjoly's 1988 speech before IEEE's professional activities section in Phoenix was typical of how most professional organizations view him. "It very deeply moved a whole bunch of our members," recalls Ed Bertnolli, IEEE vice president for professional activities. "He appeared to have been ethical in his attempt to protect the public, and he kind of got his head chopped off."
But Boisjoly has learned that praise is not the same thing as professional advancement. "Roger is a very talented technical person," says IEEE's Middleton, a retired engineer who worked for Bell of Pennsylvania. "He has a fine method of articulating his viewpoint. But he's such a public figure, any personnel director would have real concerns from a corporate standpoint of hiring somebody with such a high visibility. When they [whistle-blowers] go public, it obviously makes the career path a difficult one to follow."
Boisjoly says he has no regrets about the new direction his life has taken. But he says that the past few years have not been easy ones. "People have the wrong concept of what a whistle-blower is," he says. He insists that he's not a crusading radical, but he makes clear that he's not the type to run away from a problem he uncovers.
Boisjoly feels that a variety of duties during a 27-year career as an engineer should have paved the way for a good position near his new hometown of Mesa. But that hasn't been the case. In November 1988, he sent out 150 resumes to aerospace companies in Arizona. He got back one nibble. "It might have been because the industry has been down," he says, "or it might have been who I am and what I did.
"Industry is very reticent of hiring someone who has a mind of his own," he says. "After eight months [of waiting], I figured, `Why kid myself?' " He had spent the summer boning up in Florida for the professional engineering exams, which he took in October. Last March he was certified to set up his own company.
What hurts more than the lack of a good job is the realization that he and his wife couldn't stay in Willard. They had moved to that one-company town in 1980. They bought a house on about two acres of land with the idea that they'd settle down once he retired from Morton Thiokol. "But it was not going to be allowed to happen," he says. "Everyone was against us." Understandably, his neighbors were worried that his crusade would jeopardize their own livelihoods.
So far, those fears are unfounded. The economic outlook for Willard appears bright. Morton Thiokol has six shuttle flights left on its $2.9 billion NASA contract for the solid rocket motors, and it's competing for the chance to build rocket motors for the next 66 shuttle flights.
As far as Morton Thiokol is concerned, the Challenger is a closed chapter in U.S. space history. The company has no official comment about either the accident or Boisjoly. Two other engineers who were prominent for a brief time after telling investigators that they had opposed their company's decision to launch have elected to stay at Morton Thiokol. One, Al McDonald, is now a vice president, and the other, Arnie Thompson, is a manager. They follow their company's lead in refusing to speculate about the impact of the Challenger accident on the company and their lives.
NASA, too, seems more concerned with looking ahead than looking back. It sent 30 people to Morton Thiokol to bolster the effort to redesign the booster rockets and to calm fears about the future.
"It was a very intense, emotional undertaking, with a lot of energy spent trying to put the bad feelings behind us," says Royce Mitchell, NASA manager for the solid rocket program. "So many people did not know what would happen in terms of their jobs, their self-respect, and their image."
Although Mitchell admits that the constant oversight during the redesign project was burdensome, he believes that the effort contributed to better rapport between all members of the team. "It got a lot of people in the habit of being open and communicating and floating problems up the line," he says. "People openly and freely discuss things that in the past I am sure were not discussed. There are multiple lines of communications that we all want to maintain."
It may still be too early to know how history will ultimately remember Roger Boisjoly. But this winter, the American Broadcasting Co. will take a stab with a made-for-television movie that chronicles the six months leading up to the shuttle disaster. Boisjoly will be played by actor Peter Boyle.
George Englund, Jr., one of the producers of "The Challenger," says that in the movie, "Boisjoly is perceived by Morton Thiokol as a kind of pain in the ass. He's both a pariah and a hero. He was perceived by some people as a hero, but he's also perceived as a Chicken Little who was constantly saying `the sky is falling.' " Boisjoly was interviewed extensively as the production was under way, and was given the script to review.
Regardless of how Boisjoly is ultimately labeled, those like IEEE's William Middleton and General Motors Corp. consultant Ron Westrum (see accompanying story), who follow professional ethics issues, say that society needs these so-called Chicken Littles. "I would encourage people to be courageous, even if the penalty is stiff," says Westrum.
He hopes Boisjoly will be an inspiration to reticent employees, such as the 300 GM engineers and managers who heard Boisjoly describe his agony as he watched the Challenger explode. "It's a very potent warning about what they may have to face if they don't stand up for what they believe in," says Westrum.
APPENDIX K:
Yes, Licensing Boards Are Cartels
The case for why Congress should get involved.
Eric Boehm|Sep. 13, 2017 9:05 am
Licensing boards are perhaps the most powerful labor institution in American history.
The best estimates available suggest that roughly 30 percent of American workers are now required to get a license from one of those quasi-government agencies before they can enter the workforce. That's about the same percentage of the workforce that was a member of a union in the 1950s, the decade when union membership peaked before falling off to about half that percentage today.
There's no debate about whether the federal government has a role to play in regulating the activities of labor unions, of course. Should Congress do something about licensing boards?
"I think federal interest in this is really important," says Rebecca Allensworth, a professor of law at Vanderbilt University.
The "dirty secret behind licensing boards," Allensworth told the House Judiciary Committee on Tuesday afternoon, is that very little of what they do resembles government activity. While growing to become the largest labor institution in American history, they have too often become a self-serving institutions that act like cartels instead of protectors of public health and safety.
In research she published last year, Allensworth looked at all 1,790 state occupational licensing boards operating in America. Of those, she found that 1,515 (85 percent) of them were required by state statute to be comprised of a majority of currently licensed professionals in the same field.
"These boards are formed, by law, as cartels," Allensworth said Tuesday.
State legislatures have increasingly outsourced professional regulation to licensing boards, and in theory that's not necessarily a bad idea. Professionals working in a given field are likely to have more expertise about what rules might be needed. But in exchange for expertise, states have created the potential for professional self-dealing.
And that's not just theoretical. It's very real. In North Carolina, for example, a board comprised by a majority of actively practicing dentists decided in 2012 to send cease-and-desist letters to kiosks offering teeth whitening services. The practice of whitening teeth, the board declared, could only be done by licensed dentists.
In that instance, the Federal Trade Commission intervened. The whole case wound up in the Supreme Court, which ruled in 2015 that licensing boards controlled by a majority of "active market participants" could not make deliberately anticompetitive rules, unless those boards were "actively supervised" by some other element of state government.
Some states have responded to the Supreme Court ruling by changing how their boards operate, but the North Carolina Board of Dental Examiners v. FTC case created more questions than answers.
That's why Congress is now getting involved. In July, Rep. Darrell Issa (R-Calif.), along with three Republican senators, introduced the Restoring Board Immunity Act to clarify how state licensing boards need to be structured in order to avoid potentially expensive lawsuits challenging boards' anticompetitive rules.
In the end, licensing issues will be settled at the state level. Issa's bill is merely intended to steer states towards potential solutions to the problems created by the 2015 Supreme Court ruling. Among other things, states would have to pass legislation requiring lawmakers to conduct comprehensive reviews of their licensing boards every five years. Those would include a cost/benefit analysis and an assessment of any new licensing rules created since the last review.
There are federalism concerns about the RBI Act. Congress would be nudging states towards certain behavior with the carrot of immunity from antitrust lawsuit. Sarah Allen, a deputy attorney general in Virginia, said Tuesday that many states might be unwilling to make the changes suggested by Issa's bill, and would perhaps rather "take their chances" in court against potential anti-trust lawsuits like the one brought against the dental board in North Carolina.
The real problem, says Allensworth, is the regulatory infrastructure that has built up over the decades. There's almost unanimous, bipartisan agreement that licensing reform must be undertaken—good luck finding many other issues where Issa agrees with something the Obama administration said—yet the number of licensing laws continues to grow and more workers than ever before must get a government-issues permission slip before going to work.
The RBI act would make licensing regulations a function of the state government, the way they should be, Allensworth said, though she had a mixed opinion of some of the bill's provisions—including one element that would make it easier for workers and businesses to take licensing boards to court over disagreements.
"I want the state to take governmental responsibility for the regulation they create," she says. "Once states know the lay of the land, they will be able to balance the competitive costs of regulations themselves."
APPENDIX L:
The Truth About Dentistry
Itʼs much less scientific—and more prone to gratuitous procedures—than you may think.
FERRIS JABR
MAY 2019 ISSUE | HEALTH
Arsh Raziuddin
Like The Atlantic's family coverage? Subscribe to The Family Weekly, our free newsletter delivered to your inbox every Saturday morning.
Email SIGN UP
I N THE EARLY 2000S Terry Mitchell’s dentist retired. For a while, Mitchell, an electrician in his 50s, stopped seeking dental care altogether. But when one of his wisdom teeth began to ache, he started looking for someone new. An
acquaintance recommended John Roger Lund, whose practice was a convenient 10-minute walk from Mitchell’s home, in San Jose, California. Lund’s practice was situated in a one-story building with clay roof tiles that housed several dental offices. The interior was a little dated, but not dingy. The waiting room was small
and the decor minimal: some plants and photos, no fish. Lund was a good- looking middle-aged guy with arched eyebrows, round glasses, and graying hair that framed a youthful face. He was charming, chatty, and upbeat. At the time, Mitchell and Lund both owned Chevrolet Chevelles, and they bonded over their mutual love of classic cars.
Lund extracted the wisdom tooth with no complications, and Mitchell began seeing him regularly. He never had any pain or new complaints, but Lund encouraged many additional treatments nonetheless. A typical person might get one or two root canals in a lifetime. In the space of seven years, Lund gave Mitchell nine root canals and just as many crowns. Mitchell’s insurance covered only a small portion of each procedure, so he paid a total of about $50,000 out of pocket. The number and cost of the treatments did not trouble him. He had no idea that it was unusual to undergo so many root canals—he thought they were just as common as fillings. The payments were spread out over a relatively long period of time. And he trusted Lund completely. He figured that if he needed the treatments, then he might as well get them before things grew worse.
Meanwhile, another of Lund’s patients was going through a similar experience. Joyce Cordi, a businesswoman in her 50s, had learned of Lund through 1-800- DENTIST. She remembers the service giving him an excellent rating. When she visited Lund for the first time, in 1999, she had never had so much as a cavity. To the best of her knowledge her teeth were perfectly healthy, although she’d had a small dental bridge installed to fix a rare congenital anomaly (she was born with one tooth trapped inside another and had had them extracted). Within a year, Lund was questioning the resilience of her bridge and telling her she needed root canals and crowns.
TheAtlantic – The Trouble With Dentistry - The Atlantic - Ferris Jabr
To hear more feature stories, see our full list or get the Audm iPhone app.
Cordi was somewhat perplexed. Why the sudden need for so many procedures after decades of good dental health? When she expressed uncertainty, she says, Lund always had an answer ready. The cavity on this tooth was in the wrong position to treat with a typical filling, he told her on one occasion. Her gums were receding, which had resulted in tooth decay, he explained during another visit. Clearly she had been grinding her teeth. And, after all, she was getting older. As a doctor’s daughter, Cordi had been raised with an especially respectful view of medical professionals. Lund was insistent, so she agreed to the procedures. Over the course of a decade, Lund gave Cordi 10 root canals and 10 crowns. He also chiseled out her bridge, replacing it with two new ones that left a conspicuous gap in her front teeth. Altogether, the work cost her about $70,000.
A masked figure looms over your recumbent body, wielding power tools and sharp metal instruments, doing things to your mouth you cannot see.
In early 2012, Lund retired. Brendon Zeidler, a young dentist looking to expand his business, bought Lund’s practice and assumed responsibility for his patients. Within a few months, Zeidler began to suspect that something was amiss. Financial records indicated that Lund had been spectacularly successful, but Zeidler was making only 10 to 25 percent of Lund’s reported earnings each month. As Zeidler met more of Lund’s former patients, he noticed a disquieting trend: Many of them had undergone extensive dental work—a much larger proportion than he would have expected. When Zeidler told them, after routine exams or cleanings, that they didn’t need any additional procedures at that time, they tended to react with surprise and concern: Was he sure? Nothing at all? Had he checked thoroughly?
In the summer, Zeidler decided to take a closer look at Lund’s career. He gathered years’ worth of dental records and bills for Lund’s patients and began to
scrutinize them, one by one. The process took him months to complete. What he uncovered was appalling.
W E HAVE A FRAUGHT RELATIONSHIP with dentists as authority figures. In casual conversation we often dismiss them as “not real doctors,” regarding them more as mechanics for the mouth. But that disdain
is tempered by fear. For more than a century, dentistry has been half-jokingly compared to torture. Surveys suggest that up to 61 percent of people are apprehensive about seeing the dentist, perhaps 15 percent are so anxious that they avoid the dentist almost entirely, and a smaller percentage have a genuine phobia requiring psychiatric intervention.
When you’re in the dentist’s chair, the power imbalance between practitioner and patient becomes palpable. A masked figure looms over your recumbent body, wielding power tools and sharp metal instruments, doing things to your mouth you cannot see, asking you questions you cannot properly answer, and judging you all the while. The experience simultaneously invokes physical danger, emotional vulnerability, and mental limpness. A cavity or receding gum line can suddenly feel like a personal failure. When a dentist declares that there is a problem, that something must be done before it’s too late, who has the courage or expertise to disagree? When he points at spectral smudges on an X- ray, how are we to know what’s true? In other medical contexts, such as a visit to a general practitioner or a cardiologist, we are fairly accustomed to seeking a second opinion before agreeing to surgery or an expensive regimen of pills with harsh side effects. But in the dentist’s office—perhaps because we both dread dental procedures and belittle their medical significance—the impulse is to comply without much consideration, to get the whole thing over with as quickly as possible.
The uneasy relationship between dentist and patient is further complicated by an unfortunate reality: Common dental procedures are not always as safe, effective,
or durable as we are meant to believe. As a profession, dentistry has not yet applied the same level of self-scrutiny as medicine, or embraced as sweeping an emphasis on scientific evidence. “We are isolated from the larger health-care system. So when evidence-based policies are being made, dentistry is often left out of the equation,” says Jane Gillette, a dentist in Bozeman, Montana, who works closely with the American Dental Association’s Center for Evidence- Based Dentistry, which was established in 2007. “We’re kind of behind the times, but increasingly we are trying to move the needle forward.”
Consider the maxim that everyone should visit the dentist twice a year for cleanings. We hear it so often, and from such a young age, that we’ve internalized it as truth. But this supposed commandment of oral health has no scientific grounding. Scholars have traced its origins to a few potential sources, including a toothpaste advertisement from the 1930s and an illustrated pamphlet from 1849 that follows the travails of a man with a severe toothache. Today, an increasing number of dentists acknowledge that adults with good oral hygiene need to see a dentist only once every 12 to 16 months.
Many standard dental treatments—to say nothing of all the recent innovations and cosmetic extravagances—are likewise not well substantiated by research. Many have never been tested in meticulous clinical trials. And the data that are available are not always reassuring.
The Cochrane organization, a highly respected arbiter of evidence-based medicine, has conducted systematic reviews of oral-health studies since 1999. In these reviews, researchers analyze the scientific literature on a particular dental intervention, focusing on the most rigorous and well-designed studies. In some cases, the findings clearly justify a given procedure. For example, dental sealants—liquid plastics painted onto the pits and grooves of teeth like nail polish —reduce tooth decay in children and have no known risks. (Despite this, they are not widely used, possibly because they are too simple and inexpensive to earn
dentists much money.) But most of the Cochrane reviews reach one of two disheartening conclusions: Either the available evidence fails to confirm the purported benefits of a given dental intervention, or there is simply not enough research to say anything substantive one way or another.
Fluoridation of drinking water seems to help reduce tooth decay in children, but there is insufficient evidence that it does the same for adults. Some data suggest that regular flossing, in addition to brushing, mitigates gum disease, but there is only “weak, very unreliable” evidence that it combats plaque. As for common but invasive dental procedures, an increasing number of dentists question the tradition of prophylactic wisdom-teeth removal; often, the safer choice is to monitor unproblematic teeth for any worrying developments. Little medical evidence justifies the substitution of tooth-colored resins for typical metal amalgams to fill cavities. And what limited data we have don’t clearly indicate whether it’s better to repair a root-canaled tooth with a crown or a filling. When Cochrane researchers tried to determine whether faulty metal fillings should be repaired or replaced, they could not find a single study that met their standards.
“The body of evidence for dentistry is disappointing,” says Derek Richards, the director of the Centre for Evidence-Based Dentistry at the University of Dundee, in Scotland. “Dentists tend to want to treat or intervene. They are more akin to surgeons than they are to physicians. We suffer a little from that. Everybody keeps fiddling with stuff, trying out the newest thing, but they don’t test them properly in a good-quality trial.”
The general dearth of rigorous research on dental interventions gives dentists even more leverage over their patients. Should a patient somehow muster the gumption to question an initial diagnosis and consult the scientific literature, she would probably not find much to help her. When we submit to a dentist’s examination, we are putting a great deal of trust in that dentist’s experience and intuition—and, of course, integrity.
W HEN ZEIDLER PURCHASED LUND’S PRACTICE, in February 2012, he inherited a massive collection of patients’ dental histories and bills, a mix of electronic documents, handwritten charts, and
X-rays. By August, Zeidler had decided that if anything could explain the alarmingly abundant dental work in the mouths of Lund’s patients, he would find it in those records. He spent every weekend for the next nine months examining the charts of hundreds of patients treated in the preceding five years. In a giant Excel spreadsheet, he logged every single procedure Lund had performed, so he could carry out some basic statistical analyses.
The numbers spoke for themselves. Year after year, Lund had performed certain procedures at extraordinarily high rates. Whereas a typical dentist might perform root canals on previously crowned teeth in only 3 to 7 percent of cases, Lund was performing them in 90 percent of cases. As Zeidler later alleged in court documents, Lund had performed invasive, costly, and seemingly unnecessary procedures on dozens and dozens of patients, some of whom he had been seeing for decades. Terry Mitchell and Joyce Cordi were far from alone. In fact, they had not even endured the worst of it.
Whereas medicine has reckoned with some of its own tendencies toward excessive and misguided treatment, dentistry has lagged behind.
Dental crowns were one of Lund’s most frequent treatments. A crown is a metal or ceramic cap that completely encases an injured or decayed tooth, which is first shaved to a peg so its new shell will fit. Crowns typically last 10 to 15 years. Lund not only gave his patients superfluous crowns; he also tended to replace them every five years—the minimum interval of time before insurance companies will cover the procedure again.
More than 50 of Lund’s patients also had ludicrously high numbers of root canals: 15, 20, 24. (A typical adult mouth has 32 teeth.) According to one lawsuit that has since been settled, a woman in her late 50s came to Lund with only 10 natural teeth; from 2003 to 2010, he gave her nine root canals and 12 crowns. The American Association of Endodontists claims that a root canal is a “quick, comfortable procedure” that is “very similar to a routine filling.” In truth, a root canal is a much more radical operation than a filling. It takes longer, can cause significant discomfort, and may require multiple trips to a dentist or specialist. It’s also much more costly.
[ Read: Americans are going to Juarez for cheap dental care ]
Root canals are typically used to treat infections of the pulp—the soft living core of a tooth. A dentist drills a hole through a tooth in order to access the root canals: long, narrow channels containing nerves, blood vessels, and connective tissue. The dentist then repeatedly twists skinny metal files in and out of the canals to scrape away all the living tissue, irrigates the canals with disinfectant, and packs them with a rubberlike material. The whole process usually takes one to two hours. Afterward, sometimes at a second visit, the dentist will strengthen the tooth with a filling or crown. In the rare case that infection returns, the patient must go through the whole ordeal again or consider more advanced surgery.
Zeidler noticed that nearly every time Lund gave someone a root canal, he also charged for an incision and drainage, known as an I&D. During an I&D, a dentist lances an abscess in the mouth and drains the exudate, all while the patient is awake. In some cases the dentist slips a small rubber tube into the wound, which continues to drain fluids and remains in place for a few days. I&Ds are not routine adjuncts to root canals. They should be used only to treat severe infections, which occur in a minority of cases. Yet they were extremely common in Lund’s practice. In 2009, for example, Lund billed his patients for 109 I&Ds.
Zeidler asked many of those patients about the treatments, but none of them recalled what would almost certainly have been a memorable experience.
In addition to performing scores of seemingly unnecessary procedures that could result in chronic pain, medical complications, and further operations, Lund had apparently billed patients for treatments he had never administered. Zeidler was alarmed and distressed. “We go into this profession to care for patients,” he told me. “That is why we become doctors. To find, I felt, someone was doing the exact opposite of that—it was very hard, very hard to accept that someone was willing to do that.”
Zeidler knew what he had to do next. As a dental professional, he had certain ethical obligations. He needed to confront Lund directly and give him the chance to account for all the anomalies. Even more daunting, in the absence of a credible explanation, he would have to divulge his discoveries to the patients Lund had bequeathed to him. He would have to tell them that the man to whom they had entrusted their care—some of them for two decades—had apparently deceived them for his own profit.
Arsh Raziuddin
T HE IDEA OF THE DENTIST AS POTENTIAL CHARLATAN has a long and rich history. In medieval Europe, barbers didn’t just trim hair and shave beards; they were also surgeons, performing a range of minor operations including
bloodletting, the administration of enemas, and tooth extraction. Barber surgeons, and the more specialized “tooth drawers,” would wrench, smash, and knock teeth out of people’s mouths with an intimidating metal instrument called a dental key: Imagine a chimera of a hook, a hammer, and forceps. Sometimes the results were disastrous. In the 1700s, Thomas Berdmore, King George III’s “Operator for the Teeth,” described one woman who lost “a piece of jawbone as big as a walnut and three neighbouring molars” at the hands of a local barber.
Barber surgeons came to America as early as 1636. By the 18th century, dentistry was firmly established in the colonies as a trade akin to blacksmithing (Paul Revere was an early American craftsman of artisanal dentures). Itinerant dentists moved from town to town by carriage with carts of dreaded tools in tow, temporarily setting up shop in a tavern or town square. They yanked teeth or bored into them with hand drills, filling cavities with mercury, tin, gold, or molten lead. For anesthetic, they used arsenic, nutgalls, mustard seed, leeches. Mixed in with the honest tradesmen—who genuinely believed in the therapeutic power of bloodsucking worms—were swindlers who urged their customers to have numerous teeth removed in a single sitting or charged them extra to stuff their pitted molars with homemade gunk of dubious benefit.
In the mid-19th century, a pair of American dentists began to elevate their trade to the level of a profession. From 1839 to 1840, Horace Hayden and Chapin Harris established dentistry’s first college, scientific journal, and national association. Some historical accounts claim that Hayden and Harris approached the University of Maryland’s School of Medicine about adding dental instruction to the curriculum, only to be rebuffed by the resident physicians, who declared
that dentistry was of little consequence. But no definitive proof of this encounter has ever surfaced.
Whatever happened, from that point on, “the professions of dentistry and medicine would develop along separate paths,” writes Mary Otto, a health journalist, in her recent book, Teeth. Becoming a practicing physician requires four years of medical school followed by a three-to-seven-year residency program, depending on the specialty. Dentists earn a degree in four years and, in most states, can immediately take the national board exams, get a license, and begin treating patients. (Some choose to continue training in a specialty, such as orthodontics or oral and maxillofacial surgery.) When physicians complete their residency, they typically work for a hospital, university, or large health-care organization with substantial oversight, strict ethical codes, and standardized treatment regimens. By contrast, about 80 percent of the nation’s 200,000 active dentists have individual practices, and although they are bound by a code of ethics, they typically don’t have the same level of oversight.
[ Read: Why dentistry is separate from medicine ]
Throughout history, many physicians have lamented the segregation of dentistry and medicine. Acting as though oral health is somehow divorced from one’s overall well-being is absurd; the two are inextricably linked. Oral bacteria and the toxins they produce can migrate through the bloodstream and airways, potentially damaging the heart and lungs. Poor oral health is associated with narrowing arteries, cardiovascular disease, stroke, and respiratory disease, possibly due to a complex interplay of oral microbes and the immune system. And some research suggests that gum disease can be an early sign of diabetes, indicating a relationship between sugar, oral bacteria, and chronic inflammation.
Dentistry’s academic and professional isolation has been especially detrimental to its own scientific inquiry. Most major medical associations around the world have long endorsed evidence-based medicine. The idea is to shift focus away
from intuition, anecdote, and received wisdom, and toward the conclusions of rigorous clinical research. Although the phrase evidence-based medicine was coined in 1991, the concept began taking shape in the 1960s, if not earlier (some scholars trace its origins all the way back to the 17th century). In contrast, the dental community did not begin having similar conversations until the mid- 1990s. There are dozens of journals and organizations devoted to evidence- based medicine, but only a handful devoted to evidence-based dentistry.
In the past decade, a small cohort of dentists has worked diligently to promote evidence-based dentistry, hosting workshops, publishing clinical-practice guidelines based on systematic reviews of research, and creating websites that curate useful resources. But its adoption “has been a relatively slow process,” as a 2016 commentary in the Contemporary Clinical Dentistry journal put it. Part of the problem is funding: Because dentistry is often sidelined from medicine at large, it simply does not receive as much money from the government and industry to tackle these issues. “At a recent conference, very few practitioners were even aware of the existence of evidence-based clinical guidelines,” says Elliot Abt, a professor of oral medicine at the University of Illinois. “You can publish a guideline in a journal, but passive dissemination of information is clearly not adequate for real change.”
Among other problems, dentistry’s struggle to embrace scientific inquiry has left dentists with considerable latitude to advise unnecessary procedures—whether intentionally or not. The standard euphemism for this proclivity is overtreatment. Favored procedures, many of which are elaborate and steeply priced, include root canals, the application of crowns and veneers, teeth whitening and filing, deep cleaning, gum grafts, fillings for “microcavities”—incipient lesions that do not require immediate treatment—and superfluous restorations and replacements, such as swapping old metal fillings for modern resin ones. Whereas medicine has made progress in reckoning with at least some of its own tendencies toward excessive and misguided treatment, dentistry is lagging
behind. It remains “largely focused upon surgical procedures to treat the symptoms of disease,” Mary Otto writes. “America’s dental care system continues to reward those surgical procedures far more than it does prevention.”
“Excessive diagnosis and treatment are endemic,” says Jeffrey H. Camm, a dentist of more than 35 years who wryly described his peers’ penchant for “creative diagnosis” in a 2013 commentary published by the American Dental Association. “I don’t want to be damning. I think the majority of dentists are pretty good.” But many have “this attitude of ‘Oh, here’s a spot, I’ve got to do something.’ I’ve been contacted by all kinds of practitioners who are upset because patients come in and they already have three crowns, or 12 fillings, or another dentist told them that their 2-year-old child has several cavities and needs to be sedated for the procedure.”
Trish Walraven, who worked as a dental hygienist for 25 years and now manages a dental-software company with her husband in Texas, recalls many troubling cases: “We would see patients seeking a second opinion, and they had treatment plans telling them they need eight fillings in virgin teeth. We would look at X-rays and say, ‘You’ve got to be kidding me.’ It was blatantly overtreatment—drilling into teeth that did not need it whatsoever.”
Joyce Cordi’s new dentist says her X-rays resemble those of someone who had reconstructive facial surgery following a car crash.
Studies that explicitly focus on overtreatment in dentistry are rare, but a recent field experiment provides some clues about its pervasiveness. A team of researchers at ETH Zurich, a Swiss university, asked a volunteer patient with three tiny, shallow cavities to visit 180 randomly selected dentists in Zurich. The Swiss Dental Guidelines state that such minor cavities do not require fillings;
rather, the dentist should monitor the decay and encourage the patient to brush regularly, which can reverse the damage. Despite this, 50 of the 180 dentists suggested unnecessary treatment. Their recommendations were incongruous: Collectively, the overzealous dentists singled out 13 different teeth for drilling; each advised one to six fillings. Similarly, in an investigation for Reader’s Digest, the writer William Ecenbarger visited 50 dentists in 28 states in the U.S. and received prescriptions ranging from a single crown to a full-mouth reconstruction, with the price tag starting at about $500 and going up to nearly $30,000.
A multitude of factors has conspired to create both the opportunity and the motive for widespread overtreatment in dentistry. In addition to dentistry’s seclusion from the greater medical community, its traditional emphasis on procedure rather than prevention, and its lack of rigorous self-evaluation, there are economic explanations. The financial burden of entering the profession is high and rising. In the U.S., the average debt of a dental-school graduate is more than $200,000. And then there’s the expense of finding an office, buying new equipment, and hiring staff to set up a private practice. A dentist’s income is entirely dependent on the number and type of procedures he or she performs; a routine cleaning and examination earns only a baseline fee of about $200.
In parallel with the rising cost of dental school, the amount of tooth decay in many countries’ populations has declined dramatically over the past four decades, mostly thanks to the introduction of mass-produced fluoridated toothpaste in the 1950s and ’60s. In the 1980s, with fewer genuine problems to treat, some practitioners turned to the newly flourishing industry of cosmetic dentistry, promoting elective procedures such as bleaching, teeth filing and straightening, gum lifts, and veneers. It’s easy to see how dentists, hoping to buoy their income, would be tempted to recommend frequent exams and proactive treatments—a small filling here, a new crown there—even when waiting and watching would be better. It’s equally easy to imagine how that
behavior might escalate.
“If I were to sum it up, I really think the majority of dentists are great. But for some reason we seem to drift toward this attitude of ‘I’ve got tools so I’ve got to fix something’ much too often,” says Jeffrey Camm. “Maybe it’s greed, or paying off debt, or maybe it’s someone’s training. It’s easy to lose sight of the fact that even something that seems minor, like a filling, involves removal of a human body part. It just adds to the whole idea that you go to a physician feeling bad and you walk out feeling better, but you go to a dentist feeling good and you walk out feeling bad.”
Arsh Raziuddin
I N THE SUMMER OF 2013, Zeidler asked several other dentists to review Lund’s records. They all agreed with his conclusions. The likelihood that Lund’s patients genuinely needed that many treatments was extremely low. And
there was no medical evidence to justify many of Lund’s decisions or to explain the phantom procedures. Zeidler confronted Lund about his discoveries in several face-to-face meetings. When I asked Zeidler how those meetings went, he offered a single sentence—“I decided shortly thereafter to take legal action”— and declined to comment further. (Repeated attempts were made to contact Lund and his lawyer for this story, but neither responded.)
One by one, Zeidler began to write, call, or sit down with patients who had previously been in Lund’s care, explaining what he had uncovered. They were shocked and angry. Lund had been charismatic and professional. They had assumed that his diagnoses and treatments were meant to keep them healthy. Isn’t that what doctors do? “It makes you feel like you have been violated,” Terry Mitchell says—“somebody performing stuff on your body that doesn’t need to be done.” Joyce Cordi recalls a “moment of absolute fury” when she first learned of Lund’s deceit. On top of all the needless operations, “there were all kinds of drains and things that I paid for and the insurance company paid for that never happened,” she says. “But you can’t read the dentalese.”
“A lot of them felt, How can I be so stupid? Or Why didn’t I go elsewhere?” Zeidler says. “But this is not about intellect. It’s about betrayal of trust.”
In October 2013, Zeidler sued Lund for misrepresenting his practice and breaching their contract. In the lawsuit, Zeidler and his lawyers argued that Lund’s reported practice income of $729,000 to $988,000 a year was “a result of fraudulent billing activity, billing for treatment that was unnecessary and billing for treatment which was never performed.” The suit was settled for a confidential amount. From 2014 to 2017, 10 of Lund’s former patients, including Mitchell and Cordi, sued him for a mix of fraud, deceit, battery,
financial elder abuse, and dental malpractice. They collectively reached a nearly $3 million settlement, paid out by Lund’s insurance company. (Lund did not admit to any wrongdoing.)
Lund was arrested in May 2016 and released on $250,000 bail. The Santa Clara County district attorney’s office is prosecuting a criminal case against him based on 26 counts of insurance fraud. At the time of his arraignment, he said he was innocent of all charges. The Dental Board of California is seeking to revoke or suspend Lund’s license, which is currently inactive.
Many of Lund’s former patients worry about their future health. A root canal is not a permanent fix. It requires maintenance and, in the long run, may need to be replaced with a dental implant. One of Mitchell’s root canals has already failed: The tooth fractured, and an infection developed. He said that in order to treat the infection, the tooth was extracted and he underwent a multistage procedure involving a bone graft and months of healing before an implant and a crown were fixed in place. “I don’t know how much these root canals are going to cost me down the line,” Mitchell says. “Six thousand dollars a pop for an implant —it adds up pretty quick.”
Joyce Cordi’s new dentist says her X-rays resemble those of someone who had reconstructive facial surgery following a car crash. Because Lund installed her new dental bridges improperly, one of her teeth is continually damaged by everyday chewing. “It hurts like hell,” she says. She has to wear a mouth guard every night.
What some of Lund’s former patients regret most are the psychological repercussions of his alleged duplicity: the erosion of the covenant between practitioner and patient, the germ of doubt that infects the mind. “You lose your trust,” Mitchell says. “You become cynical. I have become more that way, and I don’t like it.”
“He damaged the trust I need to have in the people who take care of me,” Cordi says. “He damaged my trust in mankind. That’s an unforgivable crime.”
This article appears in the May 2019 print edition with the headline “The Trouble With Dentistry.”
ABOUT THE AUTHOR
FERRIS JABR is a writer based in Portland, Oregon. His work has appeared in The New Yorker, The New York Times Magazine, and Scientific American.
APPENDIX M:
This article is found on the American Academy of Endodontists webpage.
My comments are in red and are supported by current research presented in my paper.
Root Canal Safety
The Truth About Endodontic Treatment and Your Health
A Consultation with Dr. Marcus Johnson
This article is endorsed by the
Dear Doctor,
I read on the internet that root canals cause cancer. Is this true?
Dear Jennifer,
Unfortunately, sources that rank high on a Google search do not always rank high on truth. So let’s set the record straight: Root canal treatment does not cause cancer or any other disease. Root canal treatment does not cause cancer or any disease. It is the residual infection in the tooth and the surrounding bone after a poorly performed root canal procedure that can be a risk factor for various systemic diseases. The fact is that root canal treatment—performed 25 million times every year by skilled dental professionals—stops infection and saves teeth. This is a misleading statement because all root canal teeth remain infected after root canal treatment and lingering infection can persist in the surrounding bone long after a root canal is completed. All root canals are NOT the same. A mediocre root canal procedure eaves abundant dead tissue and infection inside the tooth and prevents complete healing of the infection in the bone around end of the tooth root. A skilled endodontist using advanced techniques and equipment such as photo acoustic laser can perform a root canal with a much higher degree of competence than standard root canal treatment. Let’s take a closer look at what root canal treatment is, why it’s needed, and where these discredited theories come from.
Tooth Anatomy 101
A smile reveals the pearly-white crowns of your teeth. But each tooth also has one or more roots that extend down into the bone beneath your gums. In addition, there is a hollow space in the center of each tooth called the “pulp chamber” that contains living tissue (pulp). The nerves and blood vessels of the pulp pass through narrow spaces called canals, which branch from the pulp chamber and out through the root tip. Once outside the tooth, they connect with the rest of the body.
Now let’s go back to that pearly-white tooth surface you can see. This is enamel, the hardest substance in your body. It protects teeth from damage and harmful bacteria. But sometimes a tiny hole (cavity) or a crack develops in the enamel that allows bacteria to get in and begin eroding the tooth. If left alone, these bacteria may reach the pulp tissue, causing tooth destruction, inflammation and pain.
If this inflammatory process remains untreated, the pulp tissue can die off—leading to bacterial infection. An infection inside the tooth may pass through the root canals into the surrounding tissues, bone and supporting structures. This infection can result in a painful jaw abscess, and in rare cases may be life-threatening. In some cases the pain may eventually subside or go away. However, the infection won’t—even with the use of antibiotics. Removing the infection is necessary to safeguard your oral health and even your general health.
There are only a few effective treatment options to address an infected tooth: You can extract (pull) the tooth; you can get a “root canal”—shorthand for what dentists call endodontic (“endo” – inside; “odont” – tooth) treatment; or you can get an apicoectomy, a minor surgical procedure that involves cutting out the infection from the end of the root. Only endodontic treatment or apicoectomy can actually save the tooth.
Saving an Infected Tooth
Endodontic treatment involves removing inflamed, diseased pulp tissue and their byproducts, disinfecting the tooth, and then sealing the inner chamber and the canals so that bacteria will not be able to get back in. Conventional root canal treatment leaves a significant amount of dead tissue in the root canal system and does not predictably and effectively disinfect the root canal system, and porous dentin tubules. A highly skilled endodontist using photoacoustic laser technique will do a much better job at achieving total removal of dead tissue and root canal disinfection. This in turn will allow better healing of the infection in the surrounding jaw bone. This is done in a dental office, usually under local anesthesia. The tooth is then restored with a permanent filling material and often crowned (capped) to strengthen it. A root-canal-treated tooth can last decades with proper care.
Dentists who specialize in this treatment are called endodontists. They go to specialty school for an additional two years or more after dental school to learn state-of-the-art techniques, often utilizing tiny instruments, microscopes and digital imaging. They do this because they want to stop disease, not cause it!
Discredited Theories
The root (if you’ll pardon the pun) of the false assumption that endodontic treatment can cause cancer is based on false theories of an early 20th century dentist named Weston Price. He believed that leaving a “dead” organ in the body (in this case, the tooth) leads to numerous seemingly unrelated maladies. Yet getting rid of dead tissue is exactly what root canal treatment is designed to do It does NOT get rid of dead tissue. Standard root canal treatment leaves a significant amount of dead tissue in the root canal system. —with the significant bonus of keeping the tooth!
In 1951, the highly respected Journal of the American Dental Association, an evidenced-based publication, devoted an entire issue to re-examining Dr. Price’s ideas. This has been proven false. Not surprisingly, his conclusions did not hold up to the standards of modern scientific research and dental care. FALSE. The 1951 analysis by the American Dental Association is flawed and based on outdated beliefs such as bacteria detected in root canal teeth is the result of contamination. Current peer reviewed studies show the role of chronic inflammation and infection on systemic diseases, just like Price showed over 100 years ago. From that point on, endodontic procedures became the preferred method of treating salvageable infected teeth. And since then, advancements in medicine, techniques and technologies have made root canal treatment more predictable and successful than ever.
As for the risk of cancer specifically, a study published in a journal of the American Medical Association (JAMA Otolaryngology—Head & Neck Surgery) found in 2013 that cancer risk does not increase after having a root canal treatment. In fact, the study showed that dental patients with multiple endodontic treatments had a 45 percent reduced risk of cancer! NO. The article cited was not about root canals at all. The article was about how the acid produced by cavity causing bacteria and create an immune response that may lower the incidence of one type of cancer in the mouth. Not all types of cancer in all parts of the body. Most importantly, root canal teeth were only mentioned because people with a root canals tend to have a lot of cavities therefore a lot of acid producing bacteria. Root canal teeth had absolutely nothing to do with the mechanism of action. The analysis by this author is misleading and false.
This is not to say that root canal treatment doesn’t have any risks—all medical procedures do. For example, while the success rate of root canal treatment is very high, there is a risk that it won’t work the first time and the infection could return. Soreness and lingering numbness from local anesthesia are also potential risks.
Yet tooth extraction also has risks that include infection, soreness, lingering numbness and accidental damage to adjacent teeth. In addition, there is the added expense of replacing the extracted tooth if one chooses to so do.
The Choice Is Yours
The choice of whether or not to undergo root canal treatment is yours alone. It’s important to discuss all risks and benefits with your endodontist or general dentist fully so you understand your options. And in order to make an informed decision, it is essential to have the most up-to-date evidence-based information available—not discredited antiquated theories. They are not discredited theories and they are not antiquated. Interestingly, the American Dental Association cites a 1951 publication as their source in the attempt to debunk focal infection.!! But don’t look at the old research. Look at the current research. And current research is reestablishing the role of focal infection on systemic diseases. Don’t hesitate to ask your endodontist or general dentist if you would like to know more. You can also visit the website of the American Association of Endodontists for scientifically accurate information on root canal procedures. They are not a source of trusted information in my opinion.
Review Date: 7/1/2018
Authored By: Dr. Marcus Johnson
APPENDIX N:
Below is an article published in the peer reviewed journal Operative Techniques in Otolaryngology-Head and Neck Surgery where I was lead author along with two Ear Nose and Throat physicians. This article is actually one of the references cited by the AAE in the article Maxillary Sinusitis of Endodontic Origin. The surgery for this case was performed in the operating room at Putnam Hospital. I performed the surgery to remove the infected tooth and diseased bone in the upper jaw and ENT physician Gary Fishman, MD performed the sinus surgery. These are the kinds of cases that I performed while on staff at Putnam hospital.
Also below is also a fax sent to Putnam Hospital by attorney Jackson Leeds. I never met Jackson Leeds but I heard a lot about him from others who were also targeted by him. I will not get into the motives behind Jackson Leeds actions because as lawyers do what lawyers do, he may file a frivolous nuisance lawsuit against me. But suffice it to say he seemed to have been following everything that I did. Putnam hospital of course ignored his fax and nothing became of it. Atypical facial pain, or NICO as it was called, was such a very small percentage of my practice anyway and there are many peer reviewed studies supporting the treatment when properly diagnosed.
This was the minefield I was playing in. Lawyers trying to disrupt my practice with faxes like these. Internet trolls trying to get patients to sue me. A lawsuit filed against me (and others) by attorney David Wilzig in California where the plaintiff never wanted me included in the lawsuit, was happy with my treatment, and had no idea that Wilzig had sued me!!
You can read more about this case and others, Wilzig and his relationship with quackwatch and Stephen Barrett here:
https://bolenreport.com/quackbuster-attack-on-nico-flops/
https://bolenreport.com/wp-content/uploads/2016/04/Panahpour-v-Wilzig-Complaint-Stamped-1.pdf
Just a few references regarding quackwatch and Stephen Barrett.
You can google quackwatch and Stephen Barrett and decide for yourself he is a credible source, and most importantly, an objective and fair source.
https://www.sitejabber.com/reviews/quackwatch.com
http://doctorwatch.blogspot.com/2010/04/dr-ray-sahelian-md-discusses-quackwatch.html
Founder, executives of drug company guilty in conspiracy that fed opioid crisis
Reuters 4 hours ago
By Nate Raymond
BOSTON (Reuters) - The founder of Insys Therapeutics Inc on Thursday became the highest-ranking drugmaker executive convicted in a case tied to the U.S. opioid crisis, when he and four colleagues were found guilty of bribing doctors to prescribe an addictive painkiller, helping drive the epidemic.
A federal jury in Boston found John Kapoor, 75, the drugmaker's former chairman, and his co-defendants guilty of racketeering conspiracy for a scheme that also misled insurers into paying for the drug.
Kapoor's 2017 arrest came on the same day U.S. President Donald Trump declared the epidemic that has caused tens of thousands of overdose deaths annually a public health emergency.
Kapoor was found guilty of running a wide-ranging scheme to bribe doctors nationwide by retaining them to act as speakers at sham events at restaurants ostensibly meant to educate clinicians about its fentanyl spray, Subsys.
Prosecutors said Kapoor also directed efforts to defraud insurers into paying for the drug. His co-defendants include former Insys executives and managers Michael Gurry, Richard Simon, Sunrise Lee and Joseph Rowan.
John Kapoor, right, oversaw Insys’s marketing strategy of hiring doctors as seminar speakers as cover to pay them more than $1m to prescribe high doses of Subsys. (Photo: Brian Snyder/Reuters)
They face up to 20 years in prison. They denied wrongdoing, and defense lawyers signaled plans to appeal.
"Dr. Kapoor is disappointed in the verdict, as are we," Beth Wilkinson, Kapoor's lead attorney, said in a statement. "Four weeks of jury deliberations confirm that this was far from an open-and-shut case."
The U.S. Food and Drug Administration approved Subsys in 2012 only for use in treating severe cancer pain. Yet prosecutors claimed doctors who took bribes often prescribed Subsys to patients without cancer, helping boost sales for Chandler, Arizona-based Insys.
Fentanyl is an especially potent opioid, 100 times stronger than morphine.
Kapoor's lawyers acknowledged Insys paid doctors but contended he believed they were being legally paid to discuss Subsys' benefits.
Wilkinson in her opening statement in January told jurors Kapoor had no knowledge of "side deals" being cut with doctors. She said a former executive turned government witness, Alec Burlakoff, kept Kapoor in the dark about them.
Burlakoff, Insys' ex-vice president of sales, and Michael Babich, its former chief executive, testified against Kapoor after pleading guilty to participating in the scheme.
Jurors during the trial watched a rap video Insys produced for its sales staff describing its strategies that starred Burlakoff dressed as a dancing bottle of Subsys.
Witnesses also testified that Lee, an ex-stripper turned Insys regional sales director, gave a lap dance to a doctor at a Chicago club while pushing him to prescribe Subsys.
"We were expecting a different result," said Peter Horstmann, Lee's attorney. He promised to challenge the verdict.
(Reporting by Nate Raymond; Editing by Scott Malone and Bill Berkrot)