S I Goolamali, M T Carulli, U M Davies
- Correspondence to: Dr S I Goolamali, Department of Dermatology, Chelsea and Westminster Hospital, London SW10 9NH, UK E-mail: mediderm@btinternet.com
Fusobacterium nucleatum is an anaerobic bacillus of oropharyngeal origin. We describe a case of two manifestations of fusobacterium-induced sepsis originating from an asymptomatic dental root abscess.
CASE HISTORY
A 63-year-old Caucasian man presented to the accident and emergency department with a 2-week history of night sweats, anorexia, 6 kg weight loss and lumbo-sacral back pain radiating to the right buttock and thigh. In addition, he had been intermittently confused and drowsy over the previous 48 hours. Other than gout and osteoarthritis there was no significant past medical history. On examination, he was apyrexial but tachycardic, with normal cardiac sounds and no peripheral stigmata of infective endocarditis. There was no focal spinal tenderness or nuchal rigidity and neurological examination was normal apart from significantly diminished straight leg raise on the right. Laboratory tests showed raised inflammatory markers (C-reactive protein [CRP] 402 mg/L, normal range [NR]<10; erythrocyte sedimentation rate [ESR] 84 mm in first hour), leucocytosis, (total white cell count [WCC] 27.5 with neutrophils 23.1×109/L) and deranged liver function (alkaline phosphatase 282 IU/L, NR<125; AST 53 IU/L, NR<40; LDH 225 IU/L, NR<180). Serial blood cultures, myeloma screen, tumour markers, X-ray of the chest and lumbo-sacral spine, abdominal ultrasound and electrocardiogram were negative or normal. Magnetic resonance imaging of the lumbar spine showed discitis of L4/L5. This disc was subsequently aspirated under computed tomography guidance prior to commencement of empirical antibiotic therapy with intravenous flucloxacillin and oral Fucidin (sodium fusidate).
Forty-eight hours later the patient became acutely confused with signs of acute urinary retention and bilateral lower limb hypertonia and hyperreflexia. Plantar responses were flexor and muscle power normal; sensation was difficult to assess. Repeat blood tests demonstrated a rise in neutrophil count to 32.9×109/L and acute renal failure with urea 24.1 mmol/L and creatinine 409 μmol/L. Lumbar spine magnetic resonance imaging was repeated and now showed a paravertebral abscess at the L4/L5 level (Figure 1). The patient underwent urgent right L5 laminectomy with exploration of the epidural space at L4/L5 and L5/S1. Fusobacterium nucleatum was isolated from both the pus drained at operation and the original computerized tomograph-guided aspirate. Antibiotic therapy was changed to metronidazole and benzylpenicillin, to which the organism was sensitive. Urea and creatinine normalized with inotropic support and diuretics.
Following his initial recovery the patient deteriorated acutely with pyrexia and respiratory failure requiring ventilatory support. Cardiac sounds were normal, serial blood cultures remained negative and computerized tomograph of the brain was normal. Echocardiography revealed vegetations on the mitral valve indicative of infective endocarditis and gentamicin therapy was added.
After extubation, the patient's teeth were routinely examined and a previously undetected asymptomatic dental root abscess was found, thought to be the most likely source of the F. nucleatum. Further recovery was uneventful and he underwent elective dental treatment of the abscess. Follow up magnetic resonance imaging of the lumbar-spine two months later was normal.
COMMENT
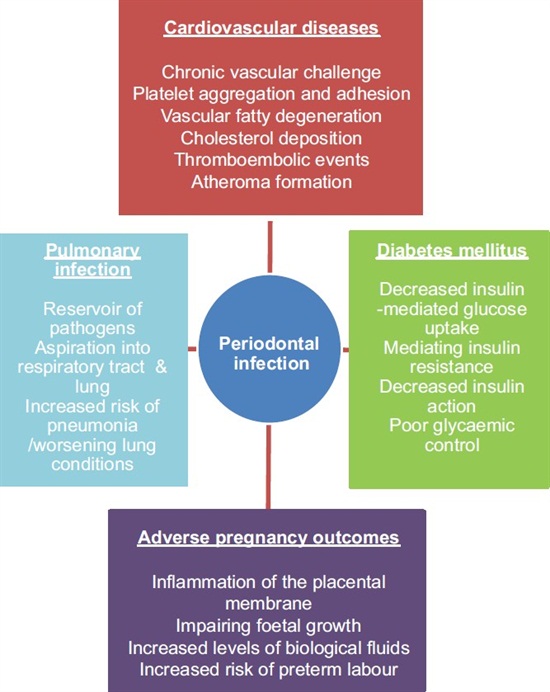
Fusobacterium spp is one of only four genera of anaerobic Gram-negative bacilli which are thought to be responsible for human infection. It produces a virulence factor liposaccharide endotoxin, which contributes to abscess formation.1 Fusobacterium nucleatum comprises part of the normal oropharyngeal bacterial flora and is a recognized pathogen in odontogenic infection. Anaerobic Gramnegative bacilli causing odontogenic orofacial infections are associated with more severe illness than other bacterial species, with F. nucleatum highlighted as a particularly potent pathogen.2 Our patient's dental root abscess, almost certainly the likely source of the bacillus, was picked up incidentally and he was entirely asymptomatic. Fusobacterium spp particularly Fusobacterium necrophorum is a recognized cause of postanginal sepsis or Lemierre's syndrome, characterized by bacteraemia with metastatic abscesses following an acute sore throat.3 It has recently been postulated that F. necrophorum is a potent pathogen and often induces the ‘simple’ sore throat in the community without co-existing sepsis.4
Anaerobic Gram-negative bacilli may frequently cause cerebral abscesses and, to a lesser extent, subdural empyemas and cranial epidural abscesses. Spinal epidural abscess is not commonly associated with these organisms:5 though acute and chronic cases can arise by haematogenous spread, either by direct seeding of the epidural space or by producing vertebral osteomyelitis (discitis) with subsequent epidural space extension. In our case, the source of infection was dental and, although the patient was on established penicillin therapy without preceding penetrating trauma or evidence of contiguous site infection, haematogenous spread was probably the mode of transmission. In the absence of any other focal infection, it is reasonable to assume that a transient bacteraemia from the dental or epidural abscess also caused the endocarditis.
Infective endocarditis caused by anaerobic bacteria is uncommon with reported incidences varying from 1%-16% of all cases.1 Bacteroides fragilis and streptococci are the most frequent causes.6 Endocarditis caused by F. nucleatum is extremely rare with only a few cases reported in the literature.7
Our patient developed focal pain for 2 weeks prior to the rapid development of radicular signs, cord compression and dissemination which forms the classic clinical presentation of an epidural abscess arising from vertebral osteomyelitis. Acute metastatic epidural space infection produces rapid progression with systemic signs of infection and localized pain predominating.1 Mortality from epidural abscess is high and early diagnosis is essential. Fusobacterium is an unusual cause for both an epidural abscess and endocarditis and emphasizes the importance of considering a spinal abscess and careful cardiac monitoring of patients complaining of focal back pain with concomitant evidence of sepsis.